In pediatrics, growth and development are two of the most basic and important assessments made of your child. Growth is a chronicle of how your child’s body is maturing from birth to adolescence. Development is a measure of your child’s maturation in physical and psychosocial abilities. These assessments are the foundations for positive health and wellness. Next month’s blog will have more information about development. For now, let’s uncover growth.
Growth is the progression of the size of the maturing human. It is measured even prior to birth to ensure the fetus is mature enough to survive outside of its mother, both in being large enough and not too large for the birth process. A fetus that is too small or too large can be indicative of health problems that are already happening prior to the birth of the baby.
Parents can follow growth along with their physician. Parenting websites provide all sorts of information about the size of a fetus from a pinpoint to walnut size to eggplant to birth. Each week, the average size of the fetus is related to a common object to which people can relate, most typically a food item. When you visit your doctor, physical measurements of the abdomen can more accurately assess growth progress. Ultrasound testing can provide quite an accurate measurement of size as well as the development and function of organs.
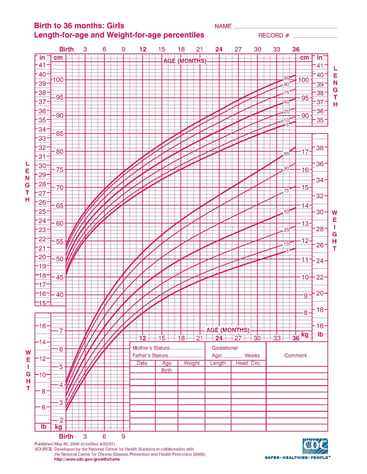
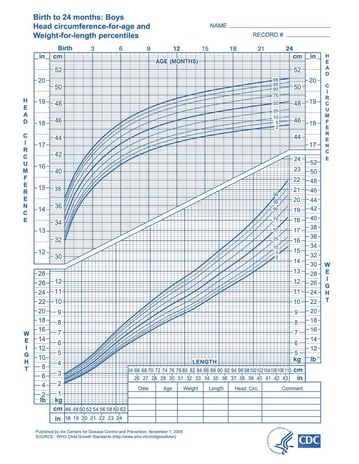
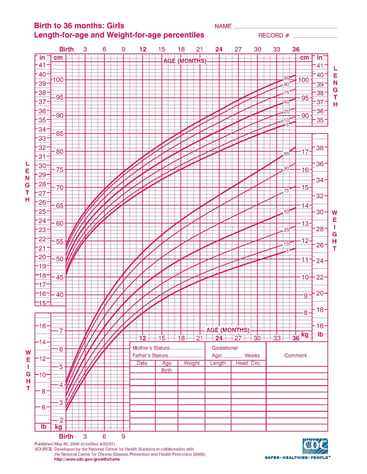
Once a baby is born, head circumference, height, and weight measurements are assessed at every doctor visit. Height and weight assessments are made throughout a person’s lifetime. Head circumference is assessed until the skull bones are fused at about age two. In the pediatric years, the measurements are placed on growth graphs. These graphs have been created using years and years of data for children with percentiles that indicate if you are on track, a little above or below average or greatly above or below average.
It is not so much if your child is in the average category as it is important to understand if your child is in the place where they should be overtime. One baby might be consistently in the lower percentile but if you look at the parents and they are very small in stature, it would be natural to think that baby will be also. If you look at the parents and find them to be very tall, the baby probably will be as well putting them in a higher percentile. Just because there is a 50% mark, does not mean your child has to land right on it.
Variability will occur as well. You might have an assessment with your child in a higher category at one visit and a lower category at another. This could be simply due to a growth spurt at the first visit and a slower growth period in the second. It is over time that should be assessed, not just one point.
 Other information should be provided to the healthcare professional at the time of growth measurement. Important information that you should talk about includes if your child has been temporarily ill, is not eating well for a health reason or has had a change in activity level. This information can help with the assessment of growth. The measurements of height and weight tell just a part of the story. Understanding the life, eating habits, and activity level provide a tremendous amount of information.
Other information should be provided to the healthcare professional at the time of growth measurement. Important information that you should talk about includes if your child has been temporarily ill, is not eating well for a health reason or has had a change in activity level. This information can help with the assessment of growth. The measurements of height and weight tell just a part of the story. Understanding the life, eating habits, and activity level provide a tremendous amount of information.
The growth charts look like the following pictures. There are different charts for boys and girls as the average size by gender can differ. Two different styles of charts are pictured. The choice of the style used is up to your healthcare provider. Age range can be from birth to 20 years or less as pictured in the examples.
Assessments that your healthcare professional will make include looking at the growth of the child over time. As previously mentioned, sometimes your child will be outside the average growth but is still very healthy and active. If there is a discrepancy between the weight and height of over 20%, further examination will be needed. For example, if your child is very tall but underweight, they might not be getting the nutrition needed. Overweight and shorter might indicate overfeeding.
These estimates do not mean you are doing anything incorrectly. There might be a metabolism issue brewing. For children with spinal cord injury who also have spasticity, extra energy may be used due to the spasticity. This can lead to an underweight assessment where supplemental feeding, treatment to better control the spasms or both might need to occur. Another common situation in SCI is poor eating because of an underactive bowel. If food is not being pushed along internally in the gut, a child will not feel hungry and naturally might not eat well. Helping to tailor the diet to improve bowel function will improve eating.
 Another issue can be too many calories. Overeating can occur from boredom, lack of diversion, isolation, loneliness, and many other factors. For children with SCI, tube feedings can be a huge contributor to increasing weight. The nutrition in formula feedings is mostly metabolized as opposed to home-cooked food which is not totally metabolized. Combined with inactivity, increased weight occurs. You will need to work with a dietician to create the right balance of formula to keep your child at a healthy weight while maintaining nutrition for proper brain and body development. Do not attempt to alter the formula on your own as serious consequences of brain damage, seizures, and other health risks can occur.
Another issue can be too many calories. Overeating can occur from boredom, lack of diversion, isolation, loneliness, and many other factors. For children with SCI, tube feedings can be a huge contributor to increasing weight. The nutrition in formula feedings is mostly metabolized as opposed to home-cooked food which is not totally metabolized. Combined with inactivity, increased weight occurs. You will need to work with a dietician to create the right balance of formula to keep your child at a healthy weight while maintaining nutrition for proper brain and body development. Do not attempt to alter the formula on your own as serious consequences of brain damage, seizures, and other health risks can occur.
Head circumference measurements are another part of growth. The head is measured at each physician visit up to the age of two years. The soft spots in the skull close at around 18 months. Once the soft spots close, the skull is rigid, so the head circumference is no longer measured. An enlarged or smaller head circumference is a sign that something is going on in the development of the brain or fluid surrounding the brain.

 Other information should be provided to the healthcare professional at the time of growth measurement. Important information that you should talk about includes if your child has been temporarily ill, is not eating well for a health reason or has had a change in activity level. This information can help with the assessment of growth. The measurements of height and weight tell just a part of the story. Understanding the life, eating habits, and activity level provide a tremendous amount of information.
Other information should be provided to the healthcare professional at the time of growth measurement. Important information that you should talk about includes if your child has been temporarily ill, is not eating well for a health reason or has had a change in activity level. This information can help with the assessment of growth. The measurements of height and weight tell just a part of the story. Understanding the life, eating habits, and activity level provide a tremendous amount of information.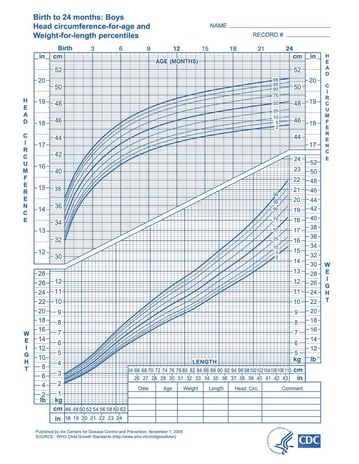 Another issue can be too many calories. Overeating can occur from boredom, lack of diversion, isolation, loneliness, and many other factors. For children with SCI, tube feedings can be a huge contributor to increasing weight. The nutrition in formula feedings is mostly metabolized as opposed to home-cooked food which is not totally metabolized. Combined with inactivity, increased weight occurs. You will need to work with a dietician to create the right balance of formula to keep your child at a healthy weight while maintaining nutrition for proper brain and body development. Do not attempt to alter the formula on your own as serious consequences of brain damage, seizures, and other health risks can occur.
Another issue can be too many calories. Overeating can occur from boredom, lack of diversion, isolation, loneliness, and many other factors. For children with SCI, tube feedings can be a huge contributor to increasing weight. The nutrition in formula feedings is mostly metabolized as opposed to home-cooked food which is not totally metabolized. Combined with inactivity, increased weight occurs. You will need to work with a dietician to create the right balance of formula to keep your child at a healthy weight while maintaining nutrition for proper brain and body development. Do not attempt to alter the formula on your own as serious consequences of brain damage, seizures, and other health risks can occur.