All the nerves in the body are important for sensation and function. Last week, the phrenic nerve was discussed because of its relationship to breathing. This week, the vagus nerve function and treatments are presented because of its importance to internal body activity, especially heart, lung, and digestive function. The word vagus means wandering in Latin. That is a good description of this nerve that travels from the brain throughout your torso as it innervates internal organs. There are some new treatments for vagus nerve function that may be of interest.
The vagus nerve is a cranial nerve which means it starts directly from within the brain. In total, there are twelve cranial nerves, and the vagus nerve is the tenth. Cranial nerves are numbered, beginning with the nerve closest to the front of the brain and moving toward the back of the brain. Since the vagus nerve is number ten, it is positioned more toward the back of the head. Cranial nerves are numbered by Roman numerals, the vagus nerve being number X (ten).
The vagus nerve has both sensory and motor functions. The sensation is provided to the outside of the body in t
he areas of skin behind the ear, the external ear canal, and parts of the throat. Inside the body, the vagus nerve provides the brain with sensations from the throat, specifically the larynx (voice box), trachea (breathing tube from the back of the mouth to the lungs), the back of the tongue, and esophagus (food tube from the back of the mouth to the stomach), the lungs, the heart, and the digestive tract. Motor function is controlled by the vagus nerve in the back of the throat as with gagging and coughing, cardiac muscles to lower resting heart rate, and peristalsis to move food through the esophagus, stomach, and intestines. In total, the vagus nerve has many functions.
Much like other parts of the body, the vagus nerve is actually two nerves that work together as a unit, so it is referred to as one nerve. It begins in the brain on the left and right sides of the medulla oblongata of the brain stem. The medulla oblongata is the connection between the brain and spinal cord. It is the part of the brain that sends messages to control most of the body’s essential functions. Injury from trauma or disease to this area of the brain can affect the function of the vagus nerve.
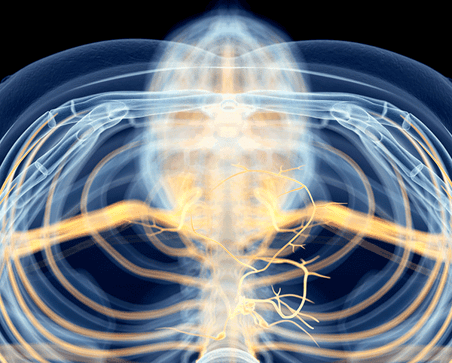
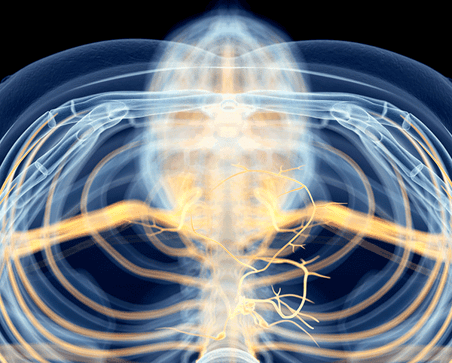
Each vagus nerve travels down the neck close to the carotid arteries and jugular vein, into the chest cavity and eventually into the abdomen. There are many branches to the vagus nerve that divide from the main nerve to provide sensation and function to the many organs listed above. At key areas, the two nerves join together in a plexus (bundle of nerves) prior to innervating the heart, lungs, liver, gallbladder, stomach, spleen, pancreas, and large and small intestines. The vagus nerve joins with the pelvic nerves the kidneys, bladder, penis, scrotum, uterus, and ovaries. Injury from trauma or disease anywhere along the main route or branches can lead to issues with sensation and function to the endpoints.
The parasympathetic nervous system controls the vagus nerve. This is the system that leads your body to rest and digest or slows the body as opposed to the sympathetic nervous system, which speeds up the body. The vagus nerve causes the resting heart rate to slow, keeping the resting pulse at 60 to 80 beats per minute. Stimulation of the vagus nerve increases activity in your body. Injury to the spinal cord can affect the function of organs controlled by the vagus nerve as well as spinal cord nerves. The slower heart rate after SCI is one example. It also affects the digestive system, which slows digestion and movement of stool through the bowel by decreasing peristalsis.
Autonomic dysreflexia is another example of nerve miscommunication. A message to the brain that something is bothering the body might not be effectively transmitted, which then does not trigger the brain to send the message to slow the body via the vagus nerve. This leads to the elevated blood pressure of AD as well as other AD symptoms.
Vasovagal syncope can occur if the vagus nerve overreacts. This occurs when systems do not align. An example is changing to a sitting position. The heart is stimulated to beat faster with head elevation, and the blood vessels in the legs do not constrict to force the blood to the brain. The lack of blood flow to the brain causes a person to temporarily pass out. Individuals with high-level spinal cord injuries may have orthostatic hypotension, which has the same body reaction. Too aggressive stimulation in the bowel program can also trigger vasovagal syncope. Some individuals need to add lubrication containing anesthetic medication inserted prior to the bowel program as well as with suppository insertion and digital stimulation to avoid vasovagal syncope. These issues are due to vagus nerve miscommunication.
There are many other issues that the vagus nerve affects. These include unusual symptoms of feeling warm, nausea, tunnel vision, ear ringing, sweating, slow or irregular heartbeat or low blood pressure. These symptoms can be from the spinal cord nerves miscommunicating with the vagus nerve. Brain-gut control of the vagus nerve has several components. In addition to the propulsion of digested food through the bowel, there is evidence that the vagus nerve serves to control microbes in the gut and has anti-inflammatory properties as well. It has an influence on depression, post-traumatic stress disorder, inflammatory bowel disease and epilepsy. There is evidence that the vagus nerve has a part in increasing the plasticity of the nervous system or the ability to help the nervous system heal itself.
Diagnosing vagus nerve disruption can be made from physical assessment. Testing of vagus nerve function varies by the location where issues are of concern. A cotton swab tapped on the back of the throat can indicate if gag function is present. That is a clue that the vagus nerve might not be working well higher in the body. Other body assessments can indicate issues with the vagus nerve, such as blood pressure, pulse, and cardiac response to exercise. Poor bowel function can indicate issues with the vagus nerve lower in the body.
Electrical stimulation is a treatment for vagus nerve issues. A vagus nerve stimulator is implanted into the body. It is much like the nerve stimulators used to improve sensation and function from other issues. An electrode is wrapped around the left vagus nerve, most typically in the neck, with a wire to a transmitter placed under the skin in the upper chest. The stimulation can be set or altered using an external device. Stimulation is generally set by a neurologist, but in some health conditions, the individual has the advantage of altering the settings as needed.
Treatment of electrical stimulation to the vagus nerve is approved for epilepsy and other seizures, and depression. Stimulation is being researched for issues such as headaches, arthritis, inflammatory bowel disease, bipolar disorder, Alzheimer’s disease, and obesity. Studies also include treatment of multiple sclerosis (MS) and spinal cord injury. In 2020, a study that vagal stimulation could possibly control blood sugar metabolism in diabetes.