Blood-Brain Barrier & The Spinal Cord - Blog - Reeve Foundation
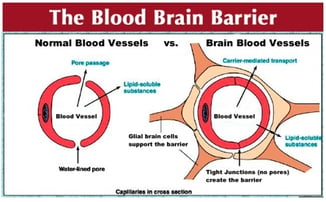
Let’s talk about the blood-brain barrier, the BBB, or as it is sometimes called, the blood-brain-spinal cord barrier. As you may recall from Biology 101, this is the physical structure, a kind of wall, that separates blood and the cerebrospinal fluid that surrounds the brain and spinal cord.
 Scientists discovered the BBB about 125 years ago, wondering why when they shot blue dye into the body all cells turned blue – except those in the brain and spinal cord. Likewise, when they shot the dye into the brain, only the brain tissue turned blue.
Scientists discovered the BBB about 125 years ago, wondering why when they shot blue dye into the body all cells turned blue – except those in the brain and spinal cord. Likewise, when they shot the dye into the brain, only the brain tissue turned blue.
The brain and spinal cord are restricted; the blood-brain barrier keeps cerebrospinal fluid extra pure and offers the central nervous system an additional layer of protection from the general flotsam and jetsum in the bloodstream.
In recent years, molecular biology has taken the BBB apart and examined it in living animals. Powerful two-photon microscopes allow visualization in real time; it’s much more complicated, of course, than anyone knew. The BBB is more like a neurovascular organ unto itself. There appears to be a tremendous amount of molecular cross-talk between the nervous system, the immune system and the cardiovascular system. And it seems the BBB itself can lead to problems. It’s being shown, for example, that a leaky BBB might be a primary culprit in several maladies, including epilepsy, Alzheimer’s disease and multiple sclerosis.
The BBB is important in spinal cord injury in two ways. First, trauma to the cord typically breaks the BBB, thus contributing to inflammation, edema and cellular mayhem at the injury site. We’ll see below how one group of scientists hopes to address BBB mediated toxicity with an cellular neuroprotective strategy.
Second, by its very nature, the BBB is quite restrictive; very few substances are allowed to cross from blood to CSF. Alcohol, heroin and cocaine get by; so do most antidepressants and sleeping aids (they are small molecules). Certain peptides are able to get past the barrier. But most drugs do not have access – but what if it were possible to sneak past the BBB, to deliver drugs to nerve cells in the central nervous system? This could be huge for nervous system cancers, for example, and also for nurturing and perhaps restoring damaged nerve cells in the brain or spinal cord.
Here we report that a group from the University of Washington has developed a way to ferry molecular cargo, including biologic drugs, to brain and spinal cord neurons. The work comes from Suzie Hwang Pun’s lab; Phil Horner, a spinal cord scientist we’ve discussed here before (he is now director of neurodegenerative medicine at Houston Methodist Research Institute) is co-principal investigator for the project. They came up with a peptide they call TAxI, short for targeted axonal import, to sort of back-door a potentially therapeutic protein into a nerve cell, without being screened and rejected by the BBB.
From a UW press release:
A study published Feb. 16 in the Proceedings of the National Academy of Sciences showed that, in mice, a muscle injection of TAxI could transport a recombinant protein into spinal motor neurons. These nerve cells are stationed within the spinal cord but extend their fibers to innervate muscles and control their movement.
"Biologic therapeutics, such as proteins or nucleic acids, are notoriously difficult to get into the central nervous system," said Pun, Professor of Bioengineering at the University of Washington and co-senior author of the work. "Our group initiated this work to develop delivery vehicles that access the spinal cord by mimicking the route some viruses and toxins take."
From the published paper:The demonstration of a nonviral-mediated delivery system demonstrates the clinical potential of this technology to develop powerful therapeutic tools to treat motor neuron diseases.
Here, we report the identification of a peptide that is trafficked into the spinal cord after intramuscular (IM) injection. We show that the peptide localizes with motor neurons after administration and can be used to carry proteins into the spinal cord via an intact motor axon that projects to the periphery. We further use this peptide ... to deliver an active enzyme into spinal cord neurons after peripheral muscle injection in mice. This TAxI peptide shows potential for clinical relevance because it also binds to motor neurons in human spinal cord.
Perhaps the most exciting aspect of our data is the demonstration of targeted delivery of a biologically active protein to the CNS and the demonstrated binding to neurons in human spinal cord. Impressively, a single injection of TAxI-Cre into the gastrocnemius led to efficient transfer of functional protein to motor neurons in the spinal cord.
From the paper:
For decades, herpes simplex viruses (HSVs) have been known to enter the CNS by retrograde axonal transport, and HSV has been engineered for remote gene transfer in animal models of disease. Engineered viruses and protein chimeras have also been used successfully in animal models to transfer therapeutic genes for conditions such as spinal cord injury, spinal muscular atrophy, chronic pain, and amyotrophic lateral sclerosis. However, virus-mediated gene therapy has been limited in clinical translation due to issues of immunogenicity, vector safety, and cost of production.
Whereas viral delivery can provide high levels of stable expression, TAxI-mediated delivery of proteins offers better control over dosing and would be better tolerated in repeat dosing regimens. Hence, TAxI-based peptide:protein chimeras offer a potential replacement of the viral methods used currently for protein delivery to the spinal cord.
Why is TAxI important? I asked Horner to speculate.I think the potential application of this technology for SCI is the possibility to directly modify active proteins in select motor neurons. Until now, we have had to use viral vectors to deliver genes and subsequently control expression. Certain viruses do travel retrogradely and can be taken up by muscle injection. What was surprising to us and unique for this peptide TAxI is that we can deliver active proteins.
So my speculation is that for SCI we may be able to inject select muscles for delivery of active proteins to motor neurons. Candidates could be optogenetic channels so that we can activate muscle groups that lack descending control. Or we may provide proteins that could induce transformative changes in the motor neurons to make them more plastic such as transcription factors that are know to induce dendrite growth.
Overall, I think TAxI opens up the possibility of a new method to target selective many cells of the brain through peptide-linked delivery which perhaps could carry less risk than a virus, not be permanent and easier to titer the delivery in clinic.
Back to the discussion of neuroprotection. Here’s one example of how the BBB might be a therapy target. The Jeff Koscis lab at Yale published a paper last year showing that injections of mesenchymal stem cells reduce the severity of experimental spinal cord injury. They’re not sure what the mechanism is but BBB leakeage was reduced and the animals got better.From the paper:
One important consequence of SCI is damage to the microvasculature and disruption of the blood spinal cord barrier (BSCB). In the present study we induced a contusive SCI at T9 in the rat and studied the effects of intravenous MSC infusion on BSCB permeability, microvascular architecture and locomotor recovery over a 10 week period.
SCI resulted in prolonged BSCB leakage that was most severe at the impact site but disseminated extensively rostral and caudal to the lesion over 6 weeks.
In MSC-treated rats, BSCB leakage was reduced ... and locomotor function improved beginning 1 week post-MSC infusion, i.e., 2 weeks post-SCI. These results suggest that intravenously delivered MSCs have important effects on reducing BSCB leakage which could contribute to their therapeutic efficacy.
Join Our Movement
What started as an idea has become a national movement. With your support, we can influence policy and inspire lasting change.
Become an Advocate