Skin Care
The skin is the largest living organ system of the body. It covers the entire exterior of the body with a few openings for the eyes, ears, nostrils, mouth, urethra, rectum and vagina in females.
The skin is the major protector of the body’s interior from the outside world. It keeps unwanted things out such as dirt and other matter, bacteria, viruses, parasites, and fungus, stands up to a moderate amount of pressure, and protects us from chemicals and radiation. Skin has a key job in regulation of the body by maintaining temperature through fluid balancing of peripheral blood vessel flow, sweat and body hair. It synthesizes and maintains vitamin D levels in the body.
Skin also has the ability of sensation. There are nerves in every part of skin that can help you perceive the outside world of heat, cold, touch and pain. It can tell your brain if something is uncomfortable outside of your body such as room temperature or too much sun that is burning you, or within your skin such as rash or goosebumps. Skin will send signals if you are too warm or cold, if something you touch is too warm or cold or if something is hurting you.
Sensation and responses of the skin are controlled by the Autonomic Nervous System (ANS), the part of the nervous system that is regulated without your control. The ANS is automatic. The skin sends messages to the brain through the Peripheral Nervous System (PNS) (the nerves throughout the body) through the spinal cord to the brain. The brain sends messages by way of the spinal cord to the PNS and back to the skin. We have no self-control over the PNS. The brain performs skin regulation based on messages sent to and from it automatically.
The skin is a helping organ by protection of the body and use of sensation. It does not have controlled movement on its own. Rather, the skin is flexible to allow movement of the bones and muscles contained within it. Natural skin has a certain amount of ‘give’ to it which accommodates the flexibility of your body.
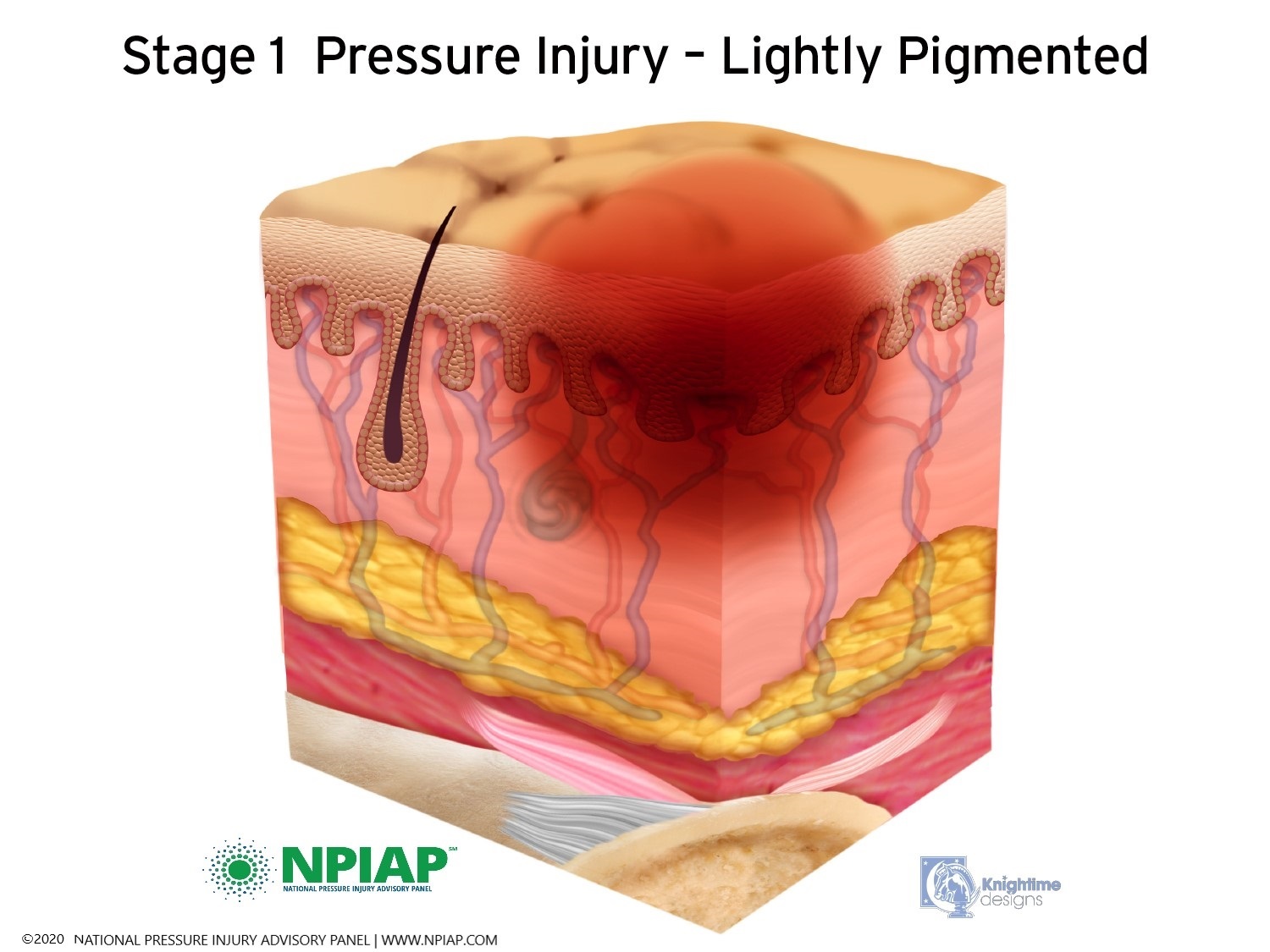
Skin is made up of two layers. The epidermis is the outer layer of skin. You can see the top of the epidermis when you look at your skin. The epidermis is a barrier that protects the inner layer of skin, the dermis. The dermis contains blood vessels, sweat glands, sebaceous glands (oil producing glands to keep the skin moist), hair follicles, nerve fibers and many small capillaries.
Just below the skin is fat (adipose) tissue which helps protect the muscles under the fat layer. Muscles are next to your bones. The muscles attach to the bones by ligaments. In the graphics below, you can see the epidermis at the top, the dermis with blood vessels, hair follicles and glands in the next layer. The yellow layer represents fat tissue. The pink layer represents muscles with the lighter pink being ligaments. White is bone.
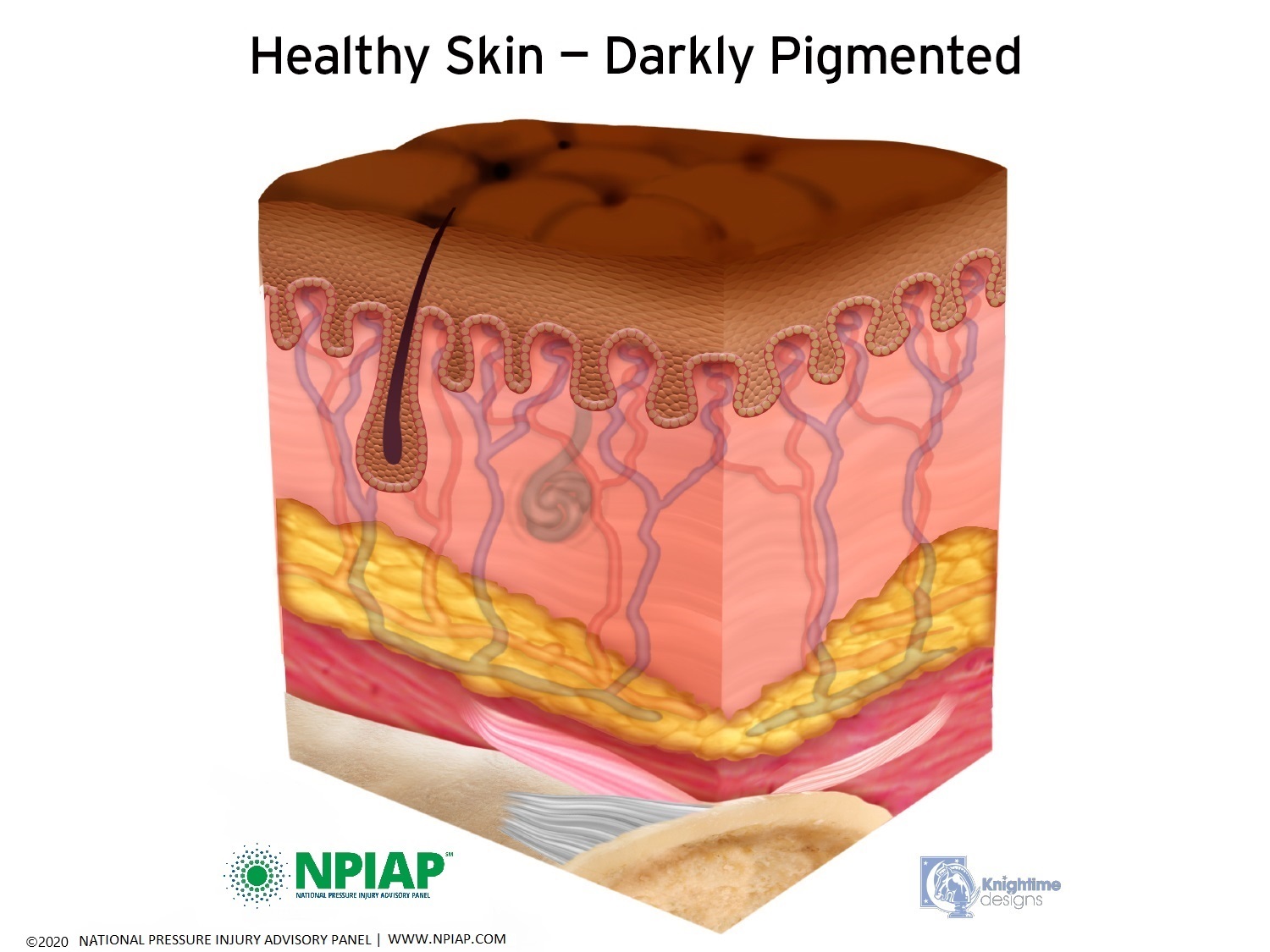
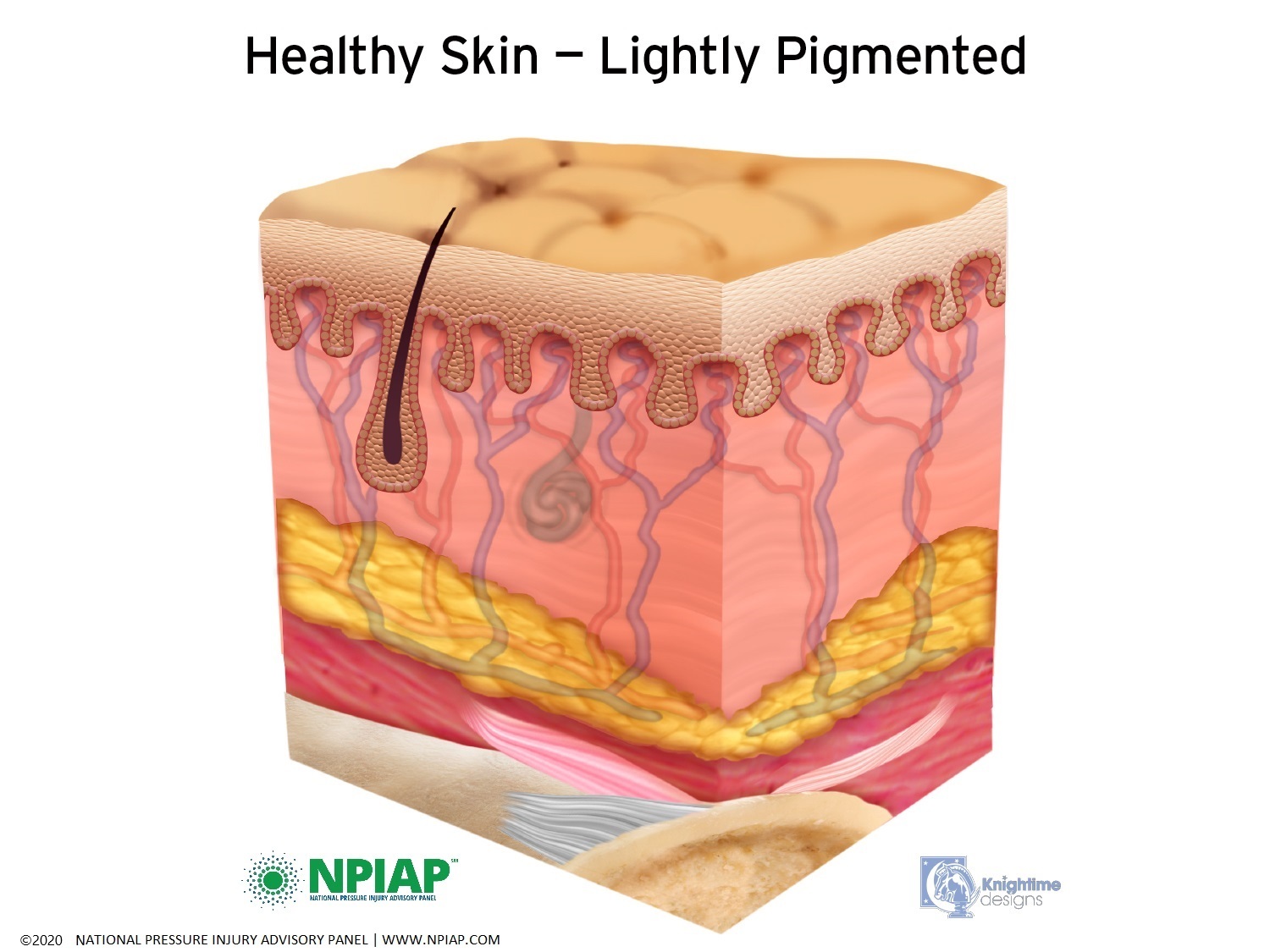
Used with permission of the National Pressure Injury Advisory Panel 11/9/20
Common skin conditions can occur to any individual. Rashes or dermatitis (derm=skin, -itis= inflammation) of all types and from all causes are extremely prevalent. Rashes can arise from an irritation on the skin from urine, feces, lotions or ointments, soap, shampoo, pollen, sweat, or something rubbing against skin. Rashes can also develop due to something taken into the body such as food, drinks, medications, or inhaled substances. A response to anxiety or stress can also produce a rash. Some common skin conditions are:
Acne typically appears on the face or back. If surgery is necessary on your back or spine but you have severe acne, the acne may need to be treated prior to the surgery to avoid internal infection.
Athlete’s foot is an itchy, red fungus typically between the toes. It occurs from sweating or wearing the same shoes daily without airing. In individuals with spinal cord injury, fungus can appear between the toes and in the folds of the skin elsewhere on the body.
Atopic Dermatitis is a long-term rash that is scaly and itches. Eczema is an example of an atopic dermatitis.
Callus is a patch of thickened skin that forms typically from something rubbing against it such as a shoe rubbing your heel, on the hands from repetitive work like propelling a wheelchair or on elbows from leaning on them or the rubbing of an assistive device. With decreased movement, calluses can form from the skin not being stimulated to slough off old skin cells.
Contact Dermatitis develops after touching or something touching you that creates red, itchy or sore skin. Assistive or positioning equipment can create a contact dermatitis.
Cancer can be benign or malignant. A rarely life-threatening skin cancer is basal cell carcinoma which is usually found on the head, neck or back. Melanoma is not a common skin cancer but well known as a malignant one. Overexposure to the sun due to a decreased ozone layer can lead to skin cancer. Not protecting your skin where you have decreased sensation can increase your risk of skin cancer.
Groin or Diaper rash occurs as a response to urine or feces on the skin. The use of plastic covered retainers for body waste that do not allow air to circulate creates an environment for bacteria to grow with or without soiled skin. It occurs in both adults and children especially with incontinence padding use, poor hygiene or within skin folds particularly while sitting.
Herpes simplex virus (HSV) includes HSV-1, cold sores and fever blisters, and HSV-2, a sexually transmitted disease.
Herpes zoster or shingles is a viral infection from dormant chicken pox. It is very painful. A rash develops on the skin following the path of a dermatome (pathway of a nerve in the body) in three days after the start of a pain or itch. There are vaccines that can reduce the incidence of having shingles or will reduce the pain and duration of the episode.
Hives is a breakout rash that appears suddenly from allergens or unknown causes.
Sunburn is a burn to the skin from sunlight. Typically, the skin turns red which is a first-degree burn. A red rash with blisters is a second-degree burn. Third- and fourth-degree sunburns have been noted. Not protecting your skin where you have decreased sensation can increase your risk of sunburn.
Psoriasis is an itchy red area with thickened skin and silvery patches. It can appear anywhere on the body but predominately appears on knees and elbows. Some individuals with psoriasis develop psoriatic arthritis.
Rosacea is a red rash with visible blood vessels that appears on the cheeks, nose, chin and sometimes forehead. It primarily affects middle aged, lightly pigmented women but can affect anyone. It should not be confused with facial blood vessel changes related to alcoholism in men and women.
Sweating
Due to issues of the Autonomic Nervous System after spinal cord injury, control of body temperature is affected because messages to regulate are not communicated effectively. The body’s ability to regulate your internal temperature can be affected by spinal cord injury. The higher the injury, the more temperature regulation is affected through sweating.
Hyperhidrosis (HH) or excessive sweating occurs in some individuals with spinal cord injury. It can occur for unknown reasons, as a symptom of autonomic dysreflexia or any disruption in the autonomic nervous system or due to a syringomyelia which is a post-injury fluid filled cyst in the spinal cord injury area. Medications for autonomic dysreflexia may curtail the excessive sweating. The medication oxybutynin has also been used successfully.
Others with SCI find they cannot sweat below the level of injury. This can cause the body to overheat due to the ability to release sweat which is the body’s natural way of cooling. Measures to prevent overheating should be undertaken. This can include use of air conditioning, fans, cool cloths, shade and wide-brimmed hats.
Friction Injury
Friction and shearing injuries can occur on skin. You might know this type of injury as a ‘rug burn’. This is caused when the epidermis and dermis become separated particularly from decreased collagen after spinal cord injury. It most often happens when moving the body or body part by dragging it across a surface rather than lifting and moving it. Friction and shearing injuries can also occur with a new piece of adaptive equipment that repeatedly rubs your skin. The friction of the surface does not allow the epidermis to move as quickly as the body thereby breaking down the delicate attachment of the two parts of the skin. Picking your body up as you move it will help prevent friction injury. Frequent skin checks should be made with new equipment.
Calluses
Calluses can form on the heels, hands, elbows and knees from lack of ability to slough off dead skin cells. Much of the skin sloughing process occurs with body movement against clothing and shoes. If you are unable to provide movement to your skin, the cells tend to stay on your body, collecting in the form of a callus. Calluses are dry and not as elastic as skin. They crack easily which can cause pain if you have sensation, autonomic dysreflexia if sensation is decreased and create an opening that allows bacteria to enter.
Reduction of calluses should be done very carefully. Reduce a callus very slowly by soaking the area with water, then ‘buffing’ the area with a towel or wash cloth. Never reduce a callus quickly or with a sharp object as the skin beneath the callus has become soft and will easily split open. If the callus is large and thick, you may want to discuss treatment with a podiatrist.
Pressure Injury
After spinal cord injury, changes occur in the skin. Collagen which gives strength to skin is decreased as is the blood supply to skin. There is also a decrease in muscle size due to immobility which is replaced by an increase in the fat layer. The perception of sensation is also decreased or absent depending on the type of spinal cord injury. These changes can cause an individual to be more susceptible to pressure injury.
Changes in the skin, blood flow, muscle composition, fat distribution and decreased sensation due to spinal cord injury provides a set up for pressure injury. Typically, the bony prominences of the skeleton rests on muscle tissue, which disperses pressure throughout the muscle. As the muscle thins, it is less able to disperse pressure. Fat tissue increases. As pressure is added to fat tissue, it condenses which creates even more pressure over the bony area. This pressure collapses blood vessels so circulation cannot be achieved. The smaller the blood vessels, as in the tiny capillaries of the skin, the quicker blood supply is decreased. Sensation would signal you to move your body to open the capillaries prior to skin damage but after spinal cord injury, that signal is decreased or absent.
Pressure injury (PI) might be called by several other names, pressure ulcer, skin breakdown, pressure sore, bed sore or decubitus ulcer. Pressure injury begins internally, where you cannot see it start. The first sign of PI might be a darkened, red or ashy spot on the skin due to the collapse of blood vessels, most commonly over a bony prominence or cartilage area. A bony prominence is typically at the end of a bone where it has a bump. For example, you can easily feel the bump of your chin bone under your skin or the bone of your elbow or knee. The outer ear and tip of the nose are made up of cartilage that is flexible but firm tissue.
Areas Especially Susceptible to Pressure Injury
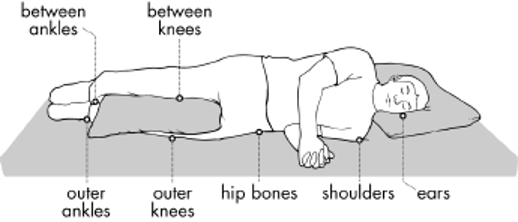
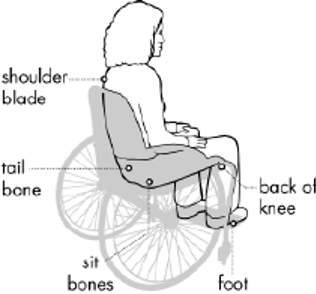
Images above appear courtesy of the Northwest Regional Spinal Cord Injury System (http://sci.washington.edu)
Pressure injury is staged by how it looks on the surface of the skin. The injury is most likely much deeper than you can see on the outside of the body.
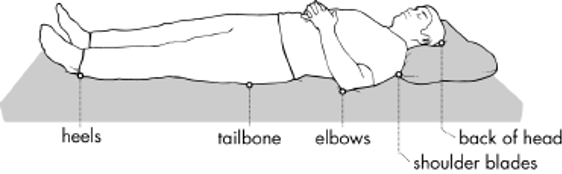
- Stage I: A pigmented area on the skin that may be painful if you have sensation. The color may vary depending on the skin tone: in darker skin, it may appear bluish or purplish; in lighter skin, the area may appear red. This is a sign that a pressure ulcer is forming. The skin may be warm or cool, firm or soft. There may be edema at the site of pigmentation and beyond.
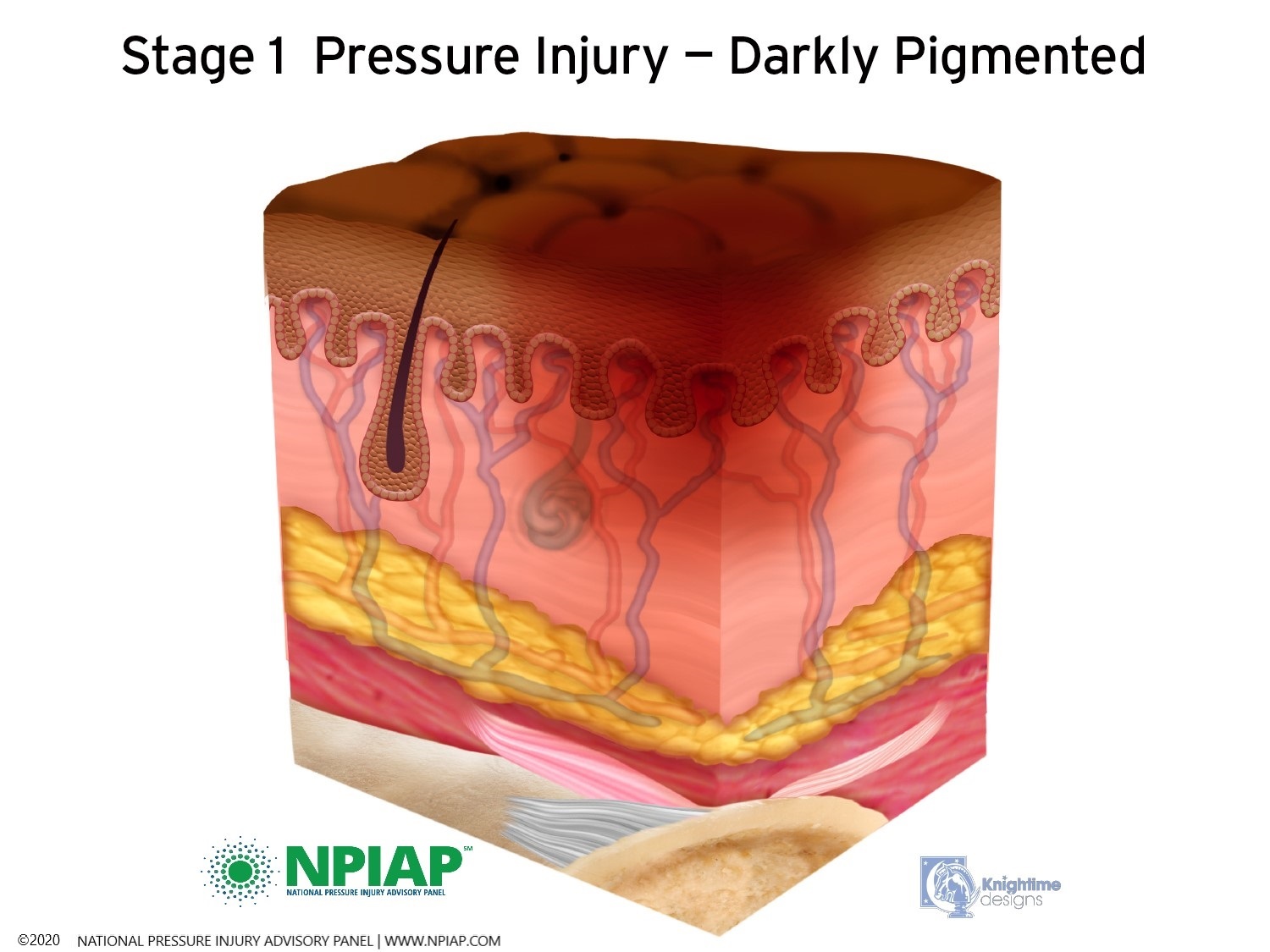
Used with permission of the National Pressure Injury Advisory Panel 11/9/20
- Stage II: The skin blisters or forms an open injury. The epidermis (top layer of skin) may be open or removed. The injury extends into the dermis. The area around the injury may be red and irritated.
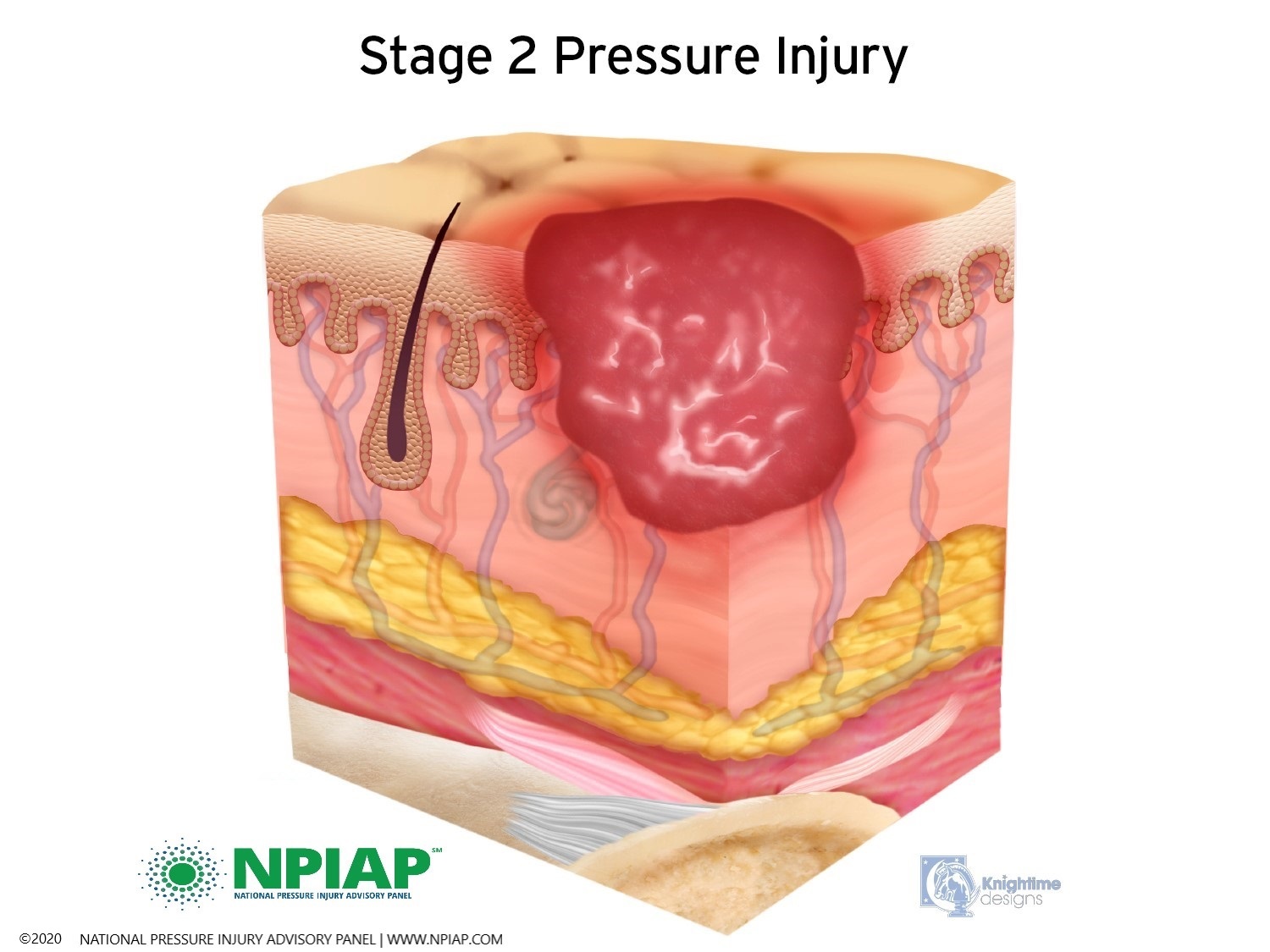
Used with permission of the National Pressure Injury Advisory Panel 11/9/20
- Stage III: The skin now develops an open, sunken hole called a crater. It extends into the body’s fat layer. Tissue below the skin is damaged. You may be able to see body fat at the bottom of the crater. There may be patches of a white substance which could be infection or decaying tissue. The edges of the opening maybe hard, lighter pigmented, and rounded inward. This is called epibole.
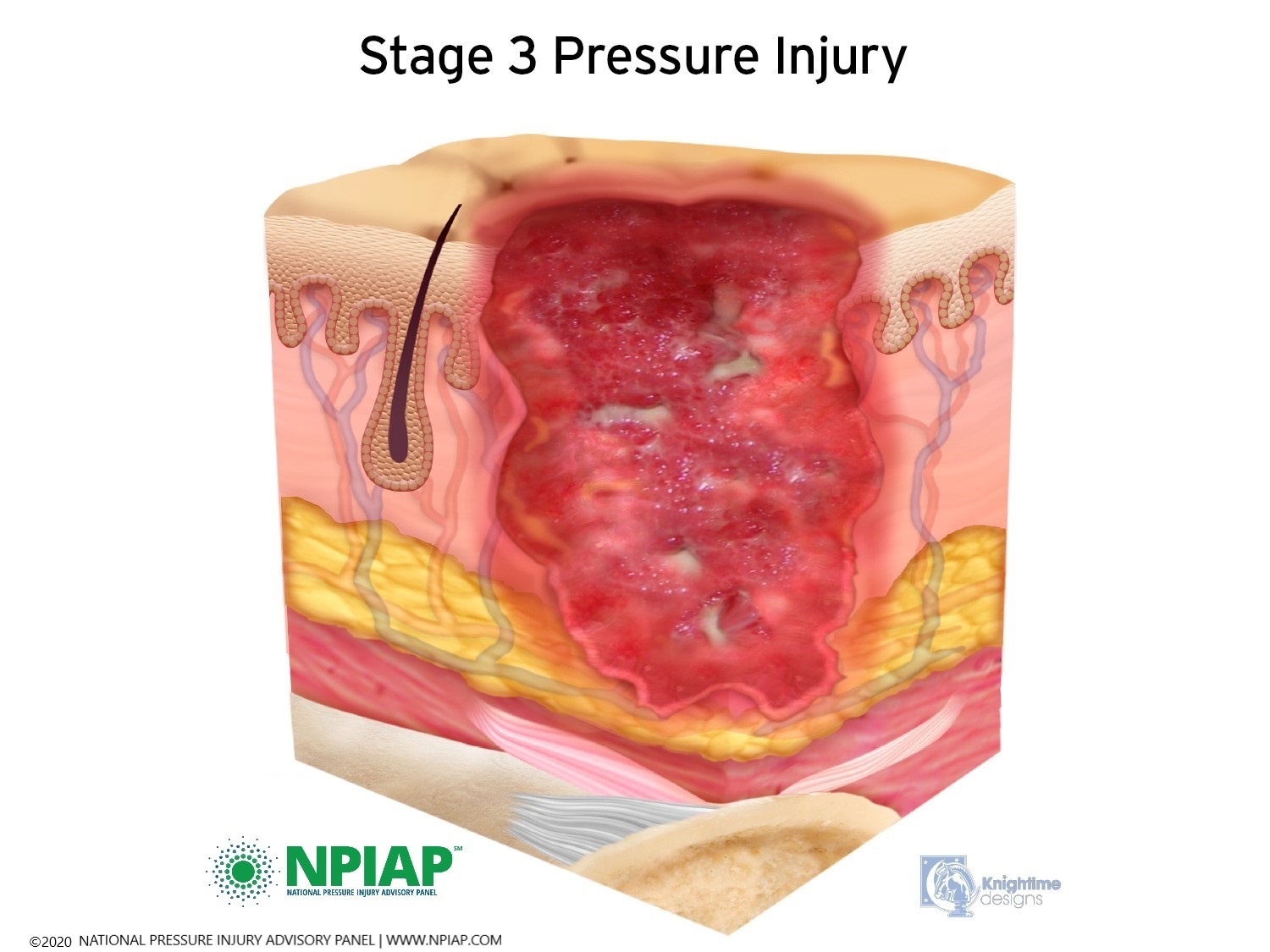
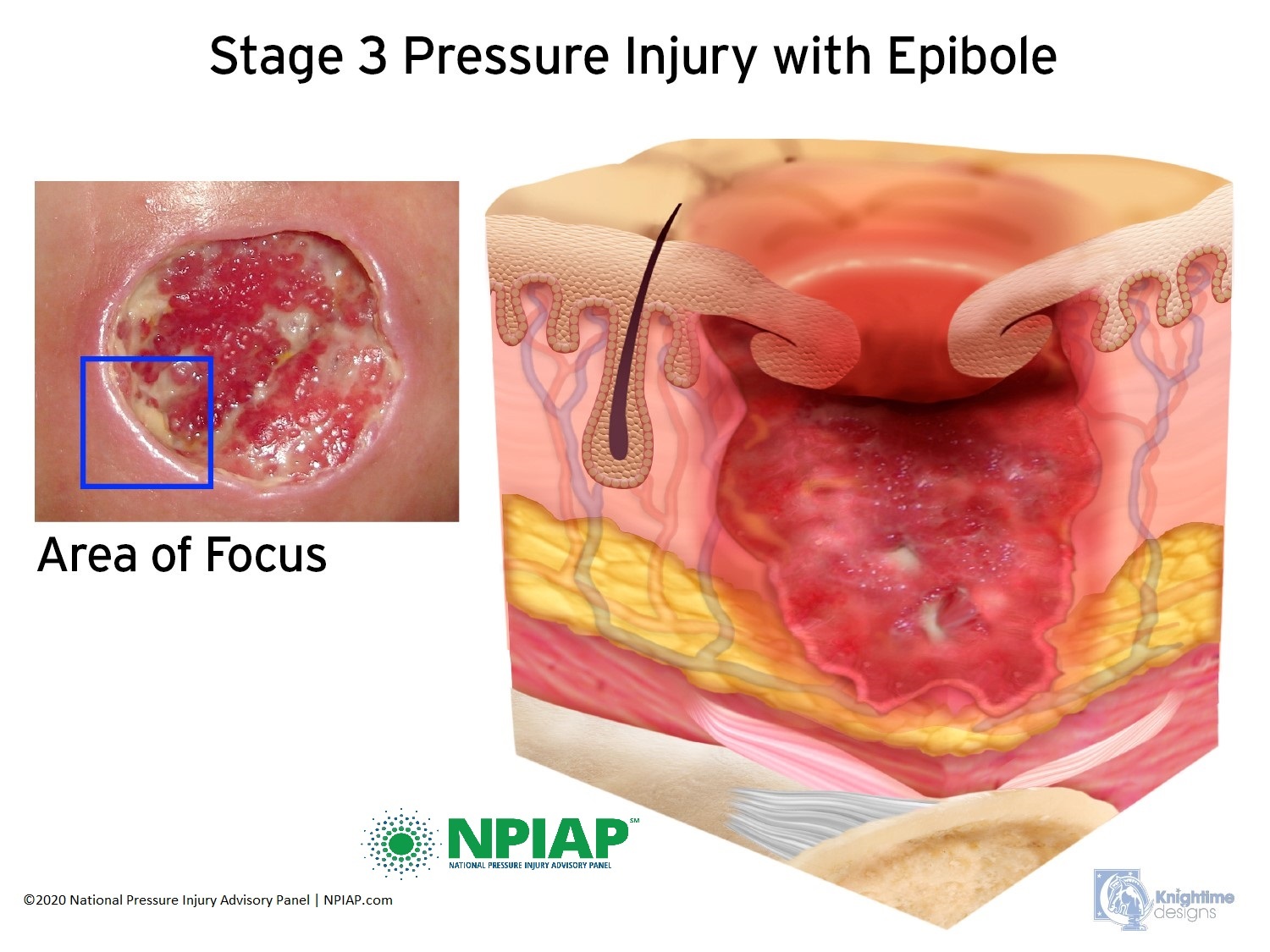
Used with permission of the National Pressure Injury Advisory Panel 11/9/20
- Stage IV: The pressure injury has reached the bone. There can be damage to the muscle and bone, and sometimes to tendons and joints.
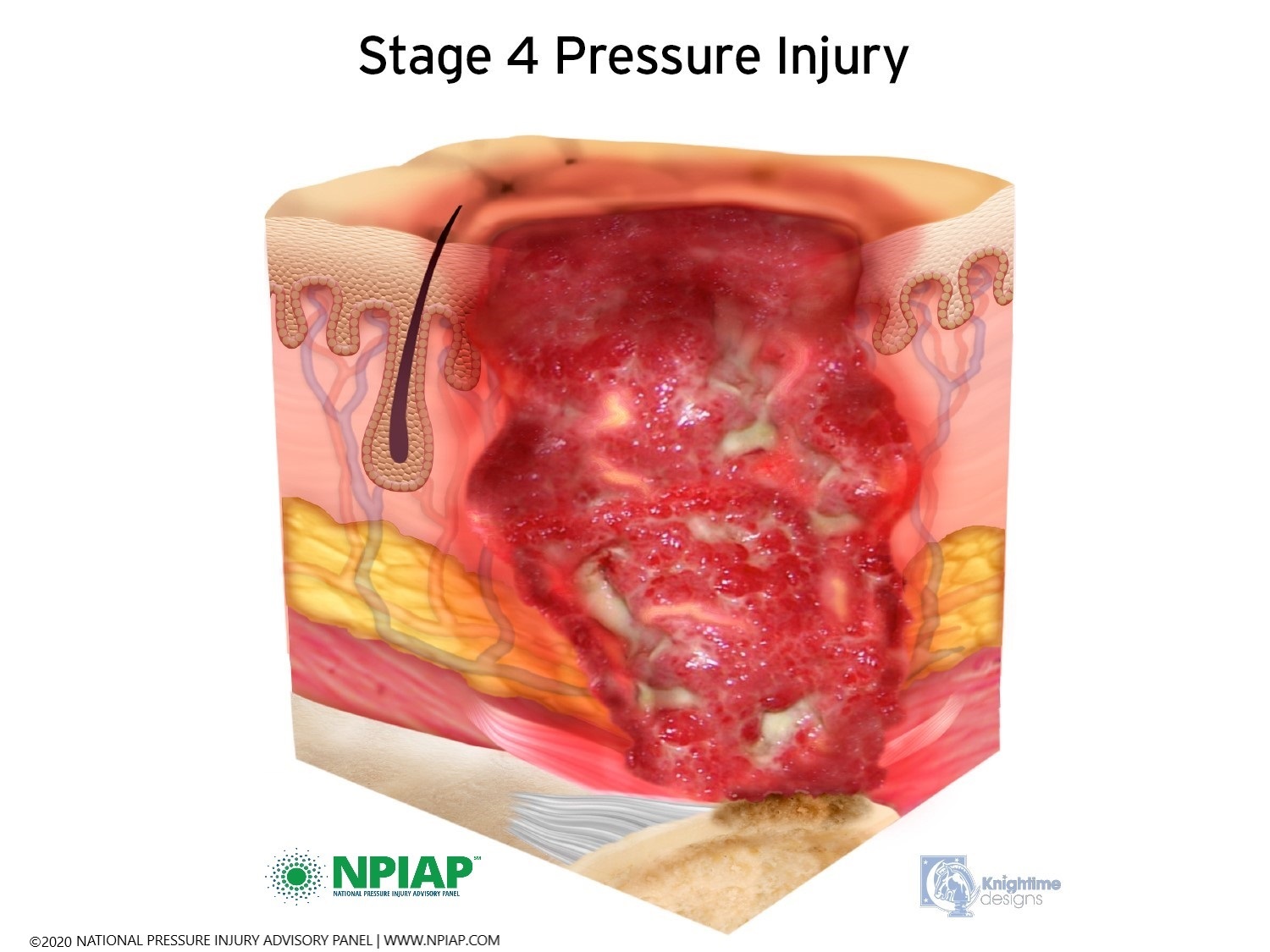
Used with permission of the National Pressure Injury Advisory Panel 11/9/20
Two other types of pressure injuries do not fit into one of the four stages.
- “Unstageable” injuries are covered in dead skin that is yellow, tan, green, or brown substance called eschar. The eschar makes it hard to assess the depth of the injury. Eschar may need to be removed by a medical professional but until it is assessed, it is keeping germs from entering the injury even though there may be infection already inside the injury that the eschar is holding in. It is important to not remove the eschar, let your medical professional determine the status of the pressure injury.
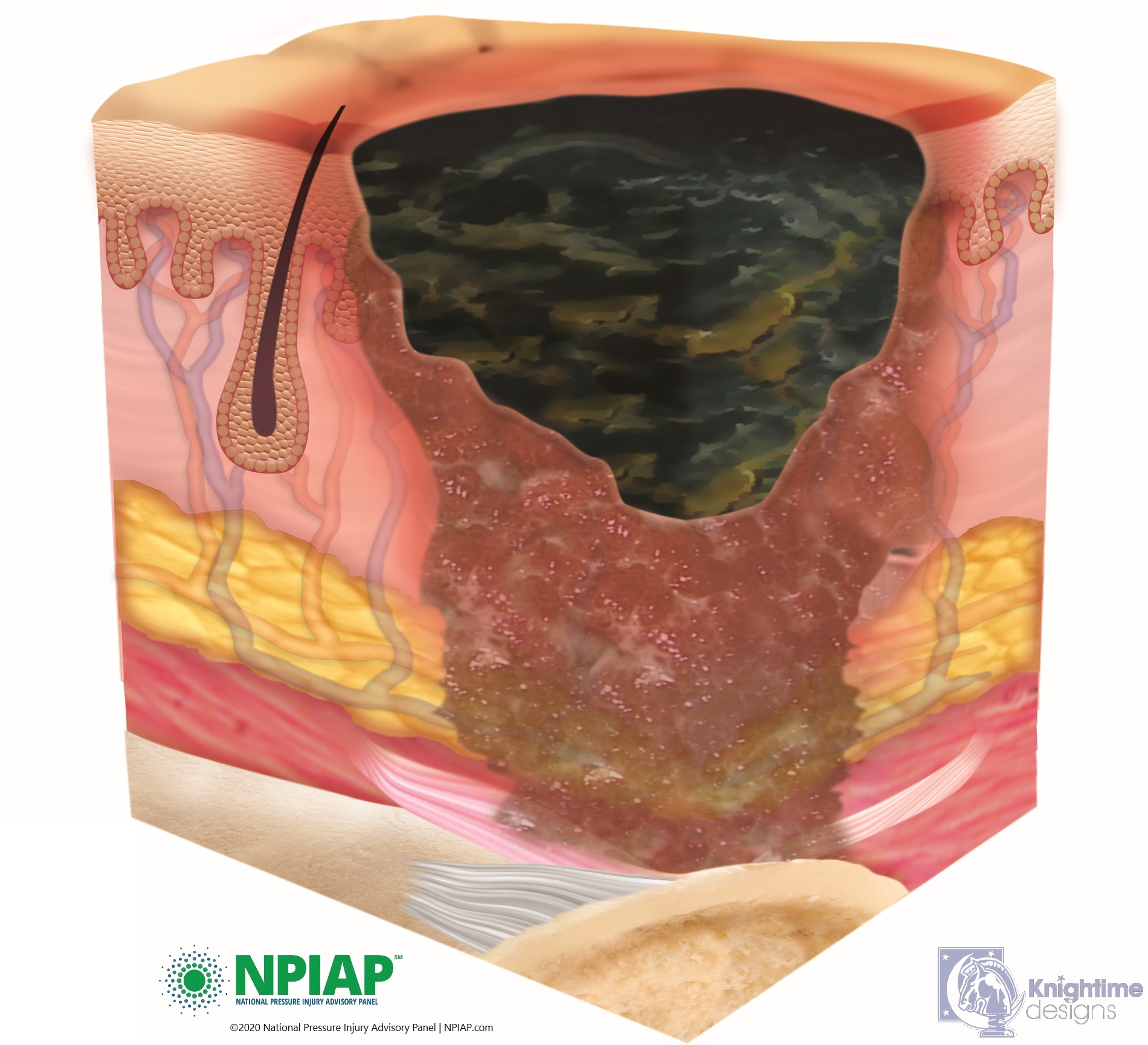
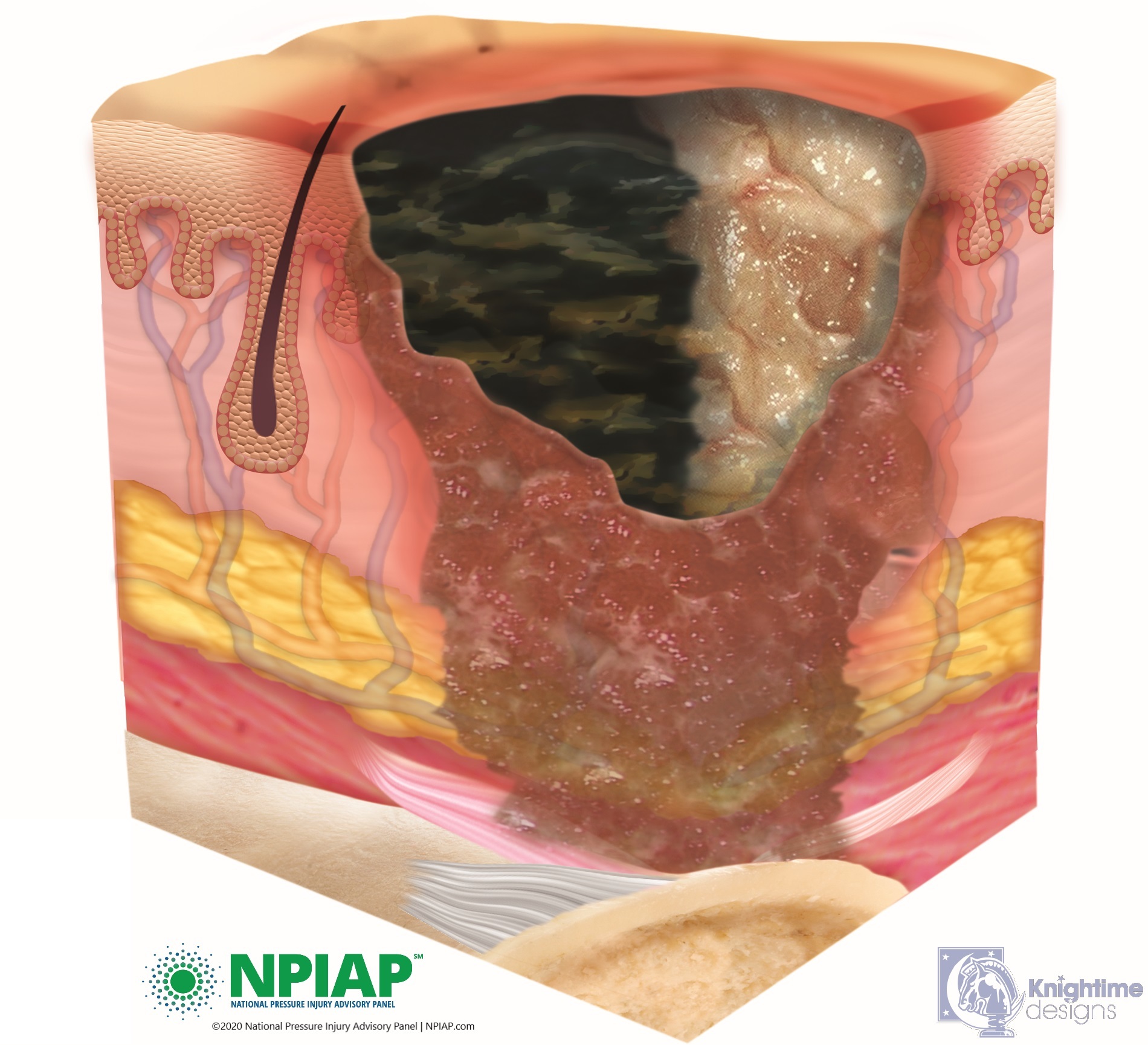
Used with permission of the National Pressure Injury Advisory Panel 11/9/20
- Pressure injuries that develop in the tissue deep below the skin are called deep tissue injuries. The area may be dark purple or maroon, and there may be a blood-filled blister under the skin. This type of skin injury can quickly become a stage III or IV pressure injury.
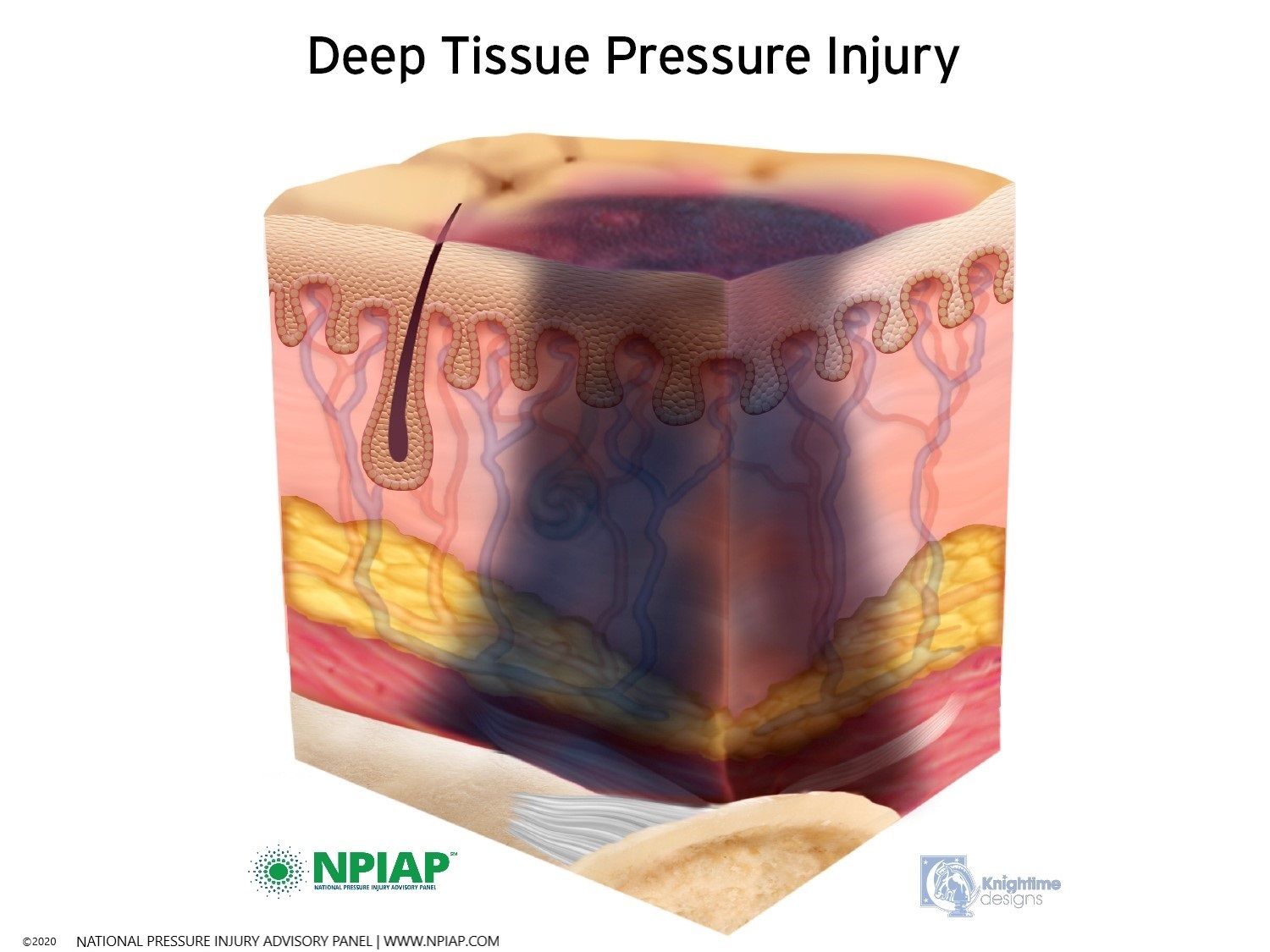
Used with permission of the National Pressure Injury Advisory Panel 11/9/20
Assessment of Pressure Injury
You are the first line of defense for your skin. Inspect your skin for rashes, calluses, open areas, changes in pigmentation, changes in temperature either cooler or warmer, cuts, tears, holes or abrasions. If you detect an issue with your skin that you do not feel can be simply treated, stay off the area and notify your healthcare professional.
Your healthcare professional will perform a physical examination with a complete assessment of your skin. Special attention will be paid to the area of possible pressure injury. Blood tests to assess for infection and nutrition might be done. If the area is open, there may be a swab of the area to assess for infection in the injury.
You will be asked about your activities of daily living (ADLs,) transferring and turning ability to lift your body rather than drag it. Frequency of pressure releases when awake or at night will be assessed. Your equipment will be evaluated to ensure it is providing the pressure dispersion, support and protection needed to maintain your skin.
For some pressure injuries where depth cannot be assessed, a CT scan or MRI might be completed to visualize the inside of the injury. This is especially important to assess if the injury has invaded the bone or is infected.
The healthcare professional possibly will complete a ‘blanch test’ of the area of pigmentation to assess blood flow. This test may not be done if the pressure injury is certain. The blanch test should only be done one time, by one healthcare professional. Additional blanch testing will not change results but will add further injury to the area. In this test, the examiner places pressure on the area with one finger, just one time. This is adding pressure so numerous tests should not be performed. If blood flow is present, the area will empty and immediately refill with blood (blanch). If blood flow is not present, there will be no change in color of the pigmented area.
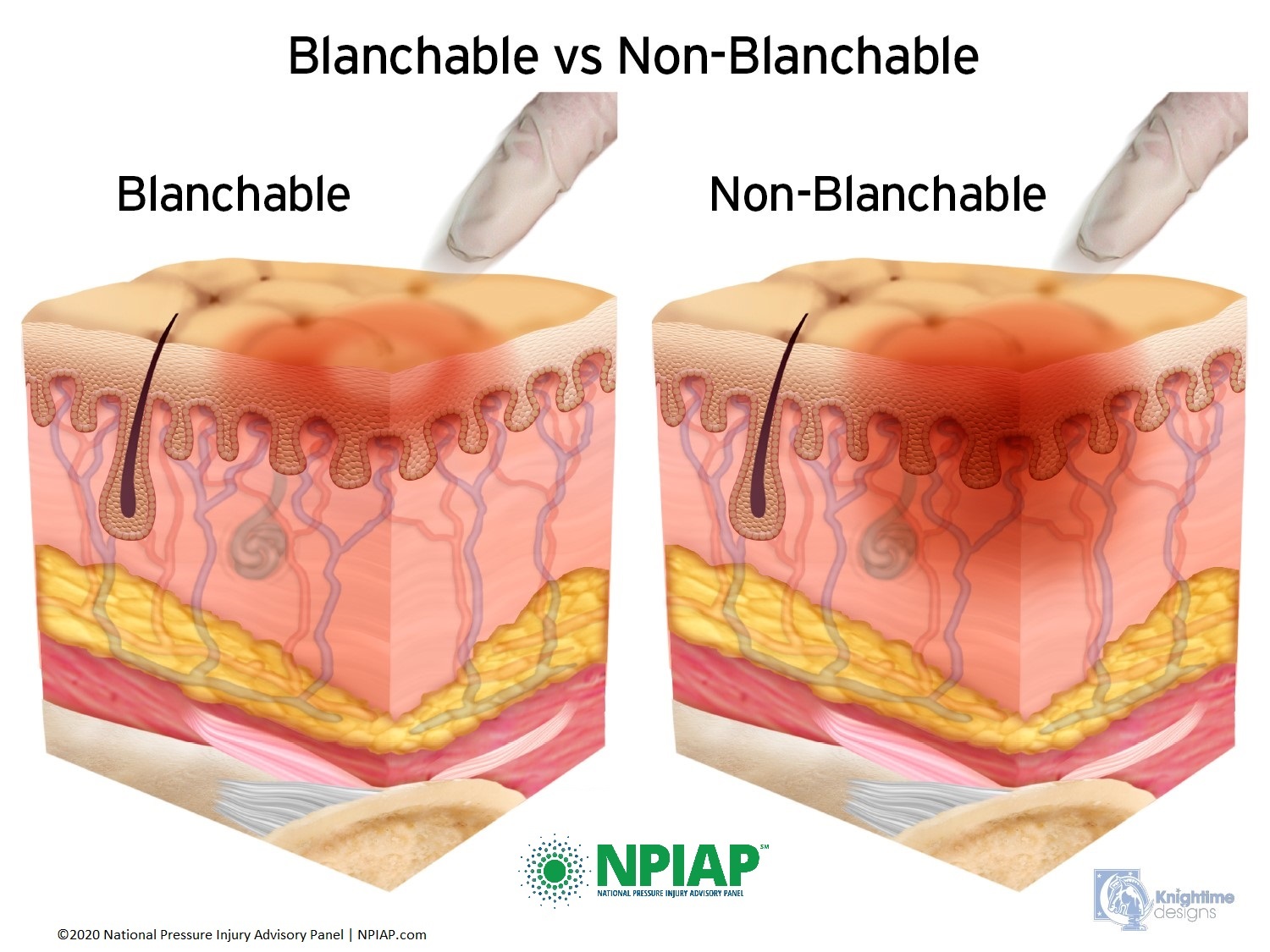
Used with permission of the National Pressure Injury Advisory Panel 11/9/20
An assessment of an open pressure injury will be made. This will include location and size (length, width, depth). The injury will be staged as indicated above. The pressure injury base, if visible will be assessed. Also noted are other characteristics such as odor, drainage, presence of blistering, slough, eschar, necrosis (dead tissue), quality of edges of the injury, and pain, increased spasticity or if autonomic dysreflexia is present or increased due to the pressure injury. A secure photo of the injury with measurement tapes will be taken. These assessments will be made by your healthcare professional or registered nurse at every visit to monitor your progress.
Some injuries have pockets or tunnels that cannot be seen due to their position within the injury. Your healthcare professional may use a sterile cotton swab to probe the opening looking for pockets or tracts which can hide bacteria or delay healing.
Treatment of Pressure Injury
Treatment of pressure injuries takes time. You may need assistance from another person to complete dressing changes or to assist you with transfers or activities of daily living. You may lose work time or family time while you are healing due to pressure restrictions.
If the skin over the pressure injury is not open, the only treatment is to stay off the area. The area of pigmentation should resolve over time. If you first notice a change in pigmentation over a bony prominence, you will need to stay completely off the area until the pigmentation returns to your usual skin color. This is non-negotiable. It means you can have no pressure on the area when laying, sitting, or other pressure on the area for any reason; not for work, school, entertainment, personal hygiene or other activity. Alternatives to your daily schedule will need to be made. If you elect to get up for just five minutes to brush your teeth, you have negated your effort of staying off the area. Often, if the pigment change has been found early, it will be just a matter of hours until the area returns to your normal color. The longer you delay offloading pressure, the longer it will take for the pigmentation to resolve.
Open injuries will require a sterile dressing to provide the protection that the skin would naturally provide as well as staying off the area. Cleaning should be done with prescribed cleansing solution or clean water. Hydrogen peroxide is NOT recommended as it destroys the granulation (formation of new cells) of the injury. Some injuries will require an irrigation to clean all aspects of the injury. Irrigation might be completed with a bulb syringe, or low-pressure irrigation device. Medication may be applied to an open injury per instructions by your healthcare provider.
Leaving a pressure injury closed by eschar can keep bacteria from entering the injury site while it heals from the injury bed up to the skin. Some pressure injuries will debride spontaneously using the body’s own immune system under an airtight dressing. Enzymes can be used with each dressing change for light debridement.
Other times, more debridement intervention is needed. This should only be completed by your healthcare professional. In the debridement process, a scalpel or chemical is used to remove eschar, necrotic tissue or tissue without circulation. Sharp (by scalpel) debridement may be done in the healthcare provider’s office with topical or local anesthetic to the area or in the operating room with general or local anesthesia. Maggot therapy has also been successful in cleaning pressure injuries.
Pressure injuries that are open typically require light packing for proper healing. Pressure injuries should be healed from the bottom of the injury first with skin closure last. The reason for this is that the skin’s job is to close to protect the body. However, if the skin closes too soon and the injury bed has not yet healed, a pocket can be formed that can reopen or become a closed festering infection. As the tissue bed heals, the packing becomes less. If there are tracts within the injury, packing should be placed in the tract for healing. Sometimes, the packing can contain medication or is placed within the injury wet. When it dries, the packing material is removed which can provide further debridement of the injury.
Some injuries require Negative Pressure Wound Therapy (NPWT). This is a device that adds a low-pressure suction to the injury which draws out drainage. There is a motorized power pack that can be placed at the bedside or on the wheelchair. Special insurance authorization is needed for this treatment.
Electrical stimulation can assist healing in Stage III or Stage IV pressure injuries. The electrical stimulation can assist in increasing blood flow to increase capillaries, oxygenation and granulation of tissue.
Hyperbaric Oxygen is a treatment sometimes offered for pressure injuries. Your entire body or body part that has a pressure injury is placed in a chamber that delivers 100% oxygen under some pressure. It is thought that the oxygen speeds healing.
Surgical closures are performed for some Stage III or Stage IV pressure injuries. Prior to surgery, nutritional status and infection must be cleared. The surgery performed removes the non-healing pressure injury area and may include reducing the bony prominence. A flap of healthy muscle is rotated to the injury area for cushioning and blood flow. The skin is closed by rotating healthy skin over the surgical site. A contract is typically signed by the patient that they will remain in bed, off the surgical area for six months to up to a year for the surgical area to heal. Then gradual seating times return with sitting for five minutes, check the area, keep pressure removed for several hours and repeat. This is a huge process that will require your total commitment to be successful.
Sepsis Pressure injuries that are infected either in the tissue, in the bone or both can become septic. This is an infection that spreads throughout your body affecting major organs. Sepsis can be fatal if not treated or not treated promptly. Sepsis is a 911 or Emergency Room situation. Symptoms of sepsis include:
Some or all the following symptoms may be present:
- Presence of infection or possible infection
- Elevated temperature, greater than 38.30C or 101.30F
- Fast heart rate, greater than 90 beats per minute
- Fast respiratory rate, greater than 20 breaths per minute
Other symptoms that maybe present:
- Confusion or coma
- Edema especially in the extremities, neck, or face
- Elevated blood sugar without diabetes
- Lower temperature below 36C or 97F
Out of date treatments for pressure injuries abound. You may find someone who recommends these, but these treatments have been debunked. The following treatments are not used today.
Massage to stimulate blood flow. Not true. Massage to a pressure injury adds more pressure causing further damage or contradicting your healthy work toward healing. Some people add the use of alcohol to stimulate blood flow during the massage. This is also adding pressure. The alcohol rub does nothing to improve blood flow.
Donut cushions. Not true. The donut forms a constriction ring around the pressure injury which decreases blood flow to the affected area.
Honey has been used off and on with the idea that the sugar content aids in pressure injury healing. There is some evidence that this does have a positive effect, but it must be medical grade honey, not from your neighbor’s hive. It also is put on the pressure injury, not eaten for healing effects.
Amputation is not the treatment for pressure injuries. An exception might be an infection in the bone that is traveling throughout your body. Clearing a pressure injury can take a long time but it does happen. Most typically, it is not an injury that requires amputation.
Maintaining Your Skin After Spinal Cord Injury
Alarms Setting reminders for pressure release is a valuable tool in maintaining a pressure release regimen. Cues can be obtained from alarm devices such as smart phones, other apps and watches. Environmental cues can be used as well for instance performing a pressure release at each cycle of television commercials or when your clock chimes each hour.
Handwashing Keeping your hands clean helps reduce the spread of infection to your body as well as to others. Wash your hands frequently with warm water and soap, using friction between your hands, for 20 seconds or the amount of time needed to sing Happy Birthday or the alphabet, twice. Hands touch many objects during the day which can pick up germs that can be spread to your body when you touch your face or catheterize. Handwashing should be done before and after doing personal hygiene tasks.
Hydration Maintaining fluid in your body keeps it working well. This includes adding moisture to your skin. Due to collagen loss after SCI, additional fluid can aid in hydrating your body including keeping your skin moist from the inside. Restrictions of fluid may be in place due to your intermittent catheterization program, cardiac issues or some types of edema. The best fluid for intake hydration is water. Water is used throughout the body. Other fluids should be used in moderation. Alcohol dehydrates the body leaving less fluid for your skin cells. Sugary and salty drinks supply an overabundance of sugar or salt which changes the ability of the body’s cells to metabolize. Be sure to check labels on fluids for sugar and salt content before drinking.
Hygiene Keeping your body clean prevents bacteria and viruses from building on the surface of the skin as well as reducing the possibility of germs from entering your body. Wash your body with warm water and a mild soap. Rinse cleanly. The friction of washing your body will help remove germs, stimulate circulation, and assists with removing old skin cells.
Bathing occurs from the top down or face first and then work down your body. The genitals followed by the gluteal fold are bathed last. An emollient lotion can provide moisture to the outside of your skin. There are many products that can be used for bathing. Some people will need a milder soap, others might prefer stronger or antibacterial soaps. Products can cause irritation for some. Be wary of products that you try especially those that cause a rash on your skin.
Moisturize Adding an emollient lotion to your skin helps add moisture from the outside of your body.
Calluses Accumulations of dead, dry skin typically appear where skin is highly used. This skin can collect from not being sloughed off by your shoes without walking, your hands from overuse like pushing a wheelchair, or from a splint or brace rubbing your skin. The callus becomes dry and cracks over time which allows bacteria to enter. Reduce a callus very slowly by soaking the area with water, then ‘buffing’ the area with a towel or wash cloth. Never reduce a callus quickly or with a sharp object as the skin beneath the callus has become soft and will easily split open. If the callus is large and thick, you may want to discuss treatment with a podiatrist.
Stop Smoking Nicotine and other substances in cigarettes, e-cigarettes, cigars, pipes, vapes and inhalants, attaches itself to red blood cells taking the place of oxygen. When you inhale nicotine or other substances, you are robbing your body of the oxygen it needs for function. This includes the skin. Talk with your healthcare professional about treatments to stop smoking. If you have done this in the past, try again. Success is possible.
Nutrition Eating a healthy and well-balanced diet is imperative in maintaining your body including skin.
Particularly needed to maintain skin and heal pressure injury are calories (or energy), protein, micronutrients (zinc, vitamin C, vitamin A, and iron), and fluids. Your caloric need has probably changed after SCI which may require less calories due to less body movement, decreased bowel function or increased calories due to spasticity. Additional nutrients may be needed to heal a pressure injury. Protein is needed to build muscles and body functioning. Micronutrients help the body perform. Each person will have individualized needs, therefore consultation with a dietician is a necessary. A nutritional assessment can help sort out your specific needs. Getting advice based on your body composition though blood testing will help you avoid over medicating yourself with nutrients that are already healthy in your body.
Weight Control Maintaining weight can be difficult after spinal cord injury. Some individuals need additional calories and others less. Being too thin can increase the risk of pressure injury as your muscles might not be meaty enough to disperse pressure from within the body even if you are using pressure reducing surfaces. Others with too much weight might be putting pressure on their body fat which compacts and does not disburse pressure. People with spinal cord injury may interpret their protruding stomach as fat when it is really due to lax stomach muscles.
Exercise Movement should be added to the parts of your body below the level of spinal cord injury in addition to body parts above the spinal cord injury. To be sure all parts of your body get movement, gently perform range of motion exercises. This stimulates blood flow which helps feed the skin, creates pressure release and improves overall body functions. If you cannot move your body, have a caregiver move it for you. If you choose to become involved with more aggressive exercise, notice if all body parts are engaged. If not, add them to your exercise regimen.
Inspection Look at your entire body a minimum of twice a day (after a night in bed and at the end of the day sitting). Skin inspection should be performed more frequently if you have a change in your health status or use new equipment or devices. If you cannot see areas of your body, use a long-handled mirror or use your phone to take a confidential photo. Monitor for any changes in pigment which could indicate a pressure injury developing or changes in your skin that could be a rash, change in oxygenation (such as a bluish tone to fingers, toes or lips) or other skin changes. This is a job that belongs to you, the owner of your skin. Caregivers change or become ill. It is critical that you know what is going on with your own body.
Pressure Reducing Surfaces Ensure you are using bed and seating surfaces that protect your entire body (including your head) anywhere sensation is decreased. Surfaces come in many types, but the goal is that they disperse pressure instead of condensing it.
There are many types of surfaces that are used for different circumstances. Bed support surfaces typically go the length of the body but the support is omitted in the head area. Instead, pillows or other pressure-reducing surfaces are used under the head because generally people have sensation there. Seating might include a surface for sitting and one for the back depending on the level of injury. Head rests, arm rests and leg rests can be selected as needed.
Pressure dispersing equipment can be made of medical grade foam (not the foam at the craft store, it does not disperse pressure) or gel. It can be air filled, fluid filled, honeycombed, or chambered so air flows from spot to spot in the device allowing less pressure under bony prominences. Mechanical devices that change pressure automatically for you also fall into this category. The selection of pressure reducing surfaces should be made with input from your healthcare professional and therapist to achieve the best match for you.
Notice this equipment is called pressure ‘reducing’ not pressure eliminating. There is no device that eliminates all pressure. Pressure releases still need to be done.
Pillows and craft foam compress and increase pressure. They are useful in holding your body in position but add pressure under bony surfaces. Nothing other than your clothes should come between you and your pressure reducing equipment.
Pressure Mapping How well your pressure reducing surface is working with your body can be measured and seen by a pressure mapping device. It is an overlay that goes between you and the pressure reducing surface you are evaluating. A picture shows how much pressure is on your bony prominences when the pressure reducing equipment is being used. A blue or green color is good, while red or orange indicates there is not enough pressure being dispersed. These are not devices that are used everyday but assessment tools that can check the status of your current equipment or new devices.
Pressure Releases To avoid pressure injury, you should perform pressure releases every 10 to 15 minutes for 60 seconds while awake. These include either holding your body up off the sitting surface, leaning from side to side, front to back or using the tilt feature on your power chair. This allows circulation to flow uninterrupted by pressure. In bed, turning every two hours or less is needed. If there is a pressure injury starting as seen by a change in skin pigmentation, stay off that area until the pigmentation change has resolved.
Positioning Maintaining body alignment is key to keeping your body most functional. This is positioning the body as it would be in a natural anatomical state. Not only does this help with breathing, digesting and blood flow but can help prevent pressure injury. Proper positioning is the natural way the body wants to be to maintain its health. It places the body in its most functional state. Careful positioning should be maintained when laying or sitting.
Shearing Move yourself by lifting your body rather than dragging it across surfaces. This eliminates shearing or the separation of the epidermis from the dermis. Shearing can be a reddened area or the epidermis can be separated leaving an open area on your skin. Even an open area in just the top layer of the skin allows bacteria to enter your body. It can also set off a pain or autonomic dysreflexia (AD) response.
Wrinkles Ensure the entire surface where there is pressure on your body is free from wrinkles. Clothing, urinary equipment, adaptive devices or other obstructions can cause pressure on your skin whether there is a bony prominence or not. Smoothing sheets and clothing keep your skin safe.
Gentleness Some individuals become rough in treatment of their bodies, mostly due to lack of sensation. We are all rushing and throwing body parts into bed or into a chair becomes habit. Be careful with your body. Gentleness can avoid many problems with skin tears, shearing, bruising, development of pressure injury, broken bones and deep vein thrombosis (DVT). You might have decreased sensation, but your body still reacts to injury and pain in other ways.
Wound Care Centers consist of experts in healing pressure injuries. If you are concerned about a pressure injury be sure to consult with the experts at a wound care center for the most up to date treatment of your injury.
Recovery from Pressure Injury
The area of a healed pressure injury is very fragile. Skin has a natural elasticity to it. This is a little ‘give’ that skin has for accommodation of pressure and movement. Skin that is a healed pressure injury is basically a scar that has no elasticity. Even if a pressure injury was surgically closed, that skin is not used to pressure. Healed or repaired skin has a greater chance of reforming a pressure injury.
Once a pressure injury has resolved, pressure tolerance begins. This starts by laying or sitting on the area for no more than 5 minutes and then being off the area for a minimum of two hours. If there is no change in pigmentation, pressure to the area is gradually increased in time on the area. Each session of pressure must be evaluated for change in pigmentation. The process continues until your normal pressure time is reached. Pressure releases must be done to accommodate the pressure even if using pressure dispersing equipment.
Because the skin over the pressure injury has less elasticity, the area will be more susceptible to future pressure injures. Be vigilant in monitoring the area.
Rehabilitation
Continued monitoring of all skin must be maintained due to decreased sensation after spinal cord injury. Keeping skin healthy is necessary for a healthy life. Those involved in care of individuals include:
Physiatrist The medical leader of your team. This doctor who specializes in physical medicine and rehabilitation directs the care needed for your healthcare situation. They may assume the care of your pressure injury or consult with other professionals.
Wound Care Physician or Plastic Surgeon Wound care physicians or plastic surgeons are medical professionals who specialize in pressure injury care. This does not mean you will have or even need surgery, but this medical specialist will prescribe the treatment needed to heal your injury.
Wound Care Nurse A registered nurse with special training will provide the treatment and dressing changes needed to heal your injury. This person will observe your pressure injury for improvement and act if healing is delayed. They will also teach you or a caregiver how to change the injury dressing at home. They will assess your equipment for providing pressure dispersion.
Physical Therapist In some areas of the country, Physical Therapists have assumed the duties of pressure injury care. The physical therapist can provide treatment to your injury as well as order equipment and teach you movement techniques to avoid further injury.
Insurance Nurse Case Manager Your insurance will provide a person to assist you with your pressure injury care needs. This is the same person assigned by your payor for your spinal cord injury care. They will work with you to get the equipment and treatments needed for resolution of your pressure injury.
Dietician After spinal cord injury, the dietician assists with ensuring you know your body’s nutritional needs for health. The dietician can assist with the caloric intake you will need as well as nutrients to increase to heal your pressure injury.
Psychologist Having a long-term pressure injury affects your life in many ways. The psychologist will help you develop strategies for dealing with a chronic problem.
Vocational Counselor Changes in your work life may be necessary for an indeterminant amount of time, especially if you are at home on bedrest. The vocational counselor can work with your employer to ensure your job continues or help you develop new skills.
Clinical Practice Guidelines are available for standards of treatment of pressure injury:
Consortium for Spinal Cord Medicine, 2014. Pressure Ulcer Prevention and Treatment Following Spinal Cord Injury: A Clinical Practice Guideline for Healthcare Professionals, 2nd Edition, Paralyzed Veterans of America. Available at no cost: www.pva.org
AWHONN. New Neonatal Skin Care Evidence‐Based Practice Guideline. Nursing for Women’s Health, Volume 17, Issue 6, December 2013–January 2014, Pages 545-546. Available for purchase: https://apps.nann.org/store/product-details?productId=59314045
The International Guideline 2019, Prevention and Treatment of Pressure Ulcer/Injuries: Clinical Practice Guidelines. Available for purchase: https://guidelinesales.com/store/viewproduct.aspx?id=15036786
Free materials for pressure injury care and equipment maintenance is available through the National Pressure Injury Advisory Panel: https://npiap.com/page/FreeMaterials
Evidence treatment of spinal cord injury pressure injury can be found at SCIRE Project: http://scireproject.com/wp-content/uploads/pressure_ulcers.pdf
Research
The study of skin and pressure injury is extensive. Skin issues are being researched in the areas of physiology (how skin functions) as well as skin illnesses such as rashes and skin healing. Artificial skin is an interest for large, open pressure injuries that can be covered to promote healing and replace the skin’s natural barrier from infection. This is especially important in the treatment of burns and pressure injury type of wounds. Research about skin is evident in the laboratory and clinical settings such as in dermatology, plastic and reconstructive surgery, physical rehabilitation, nursing and physical therapy among others.
Pressure injury is a research area that is extensive. Prevention strategies and techniques including nutrition, hydration, pressure releases, pressure dispersing equipment, and enhancement of blood flow are the key for avoiding pressure injuries. The guidelines for staging of pressure injuries have recently been revised based on current evidence (research). Injury healing treatments are considered and revisited as healthcare advances.
Specific research of pressure injury treatment include cytokine growth factor therapy (e.g. recombinant human platelet-derived growth factor (rhPDGF), basic fibroblast growth factor), cell-based therapies (platelet-rich plasma, autologous stem cell delivery), and improvements in pressure-relieving surface technology (e.g. fluid immersion technology).
Educational strategies for individuals, families, nurses and other healthcare professionals have been researched for best practice. Different educational points are stressed for the community setting, intensive and acute hospital setting and especially in the rehabilitation hospital.
Yet, with all the research in physiology, prevention and treatment, pressure injuries still occur. Often, the injuries happen even with the best of care. Finding the solution to total prevention through both human needs and mechanical issues is improving yet elusive. Because skin issues and pressure injury cross many health care issues including spinal cord injury, research is shared among healthcare professionals.
Pressure Injury Facts and Figures
In the U.S., the Collaborative Healthcare Patient Safety Organization finds Hospital Acquired Pressure Injury (HAPU) numbers 2.5 million patients. Device pressure injury is about 30% of the total number of pressure injuries.
Incidence of pressure injury of individuals with spinal cord injury is 25-66%. The higher the level of injury, the higher the incidence of pressure injury.
Worldwide 1 in 5 individuals with spinal cord injury will develop a pressure injury.
The most common areas affected by pressure injury are the sacrum (at the top of the gluteal fold, hips) and ischium (sitting bones on the bottom).
The cost of a full thickness pressure injury is estimated at $70,000 with a total of $11 billion annually.
Pressure injury is the cause of the second largest number of medical lawsuits annually at 17,000.
There are 60,000 deaths per year accounted directly to pressure injury.
Consumer Resources
If you are looking for more information about skin care and pressure injury or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm ET.
Additionally, the Reeve Foundation maintains a fact sheet about skin care and pressure injury with additional resources from trusted Reeve Foundation sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to pressure injury organizations including:
National Pressure Injury Advisory Panel https://npiap.com/
Video: Skin Care
Video: Pressure Relief
Here are a few ways to move your body in your chair to let your skin breathe and prevent pressure sores.
Further Reading
References
Alderden J, Rondinelli J, Pepper G, Cummins M, Whitney J. Risk factors for pressure injuries among critical care patients: A systematic review. International Journal of Nursing Studies, Volume 71, June 2017, pages 97-114. https://doi.org/10.1016/j.ijnurstu.2017.03.012
Bhutani S, Vishwanath G. Hyperbaric oxygen and wound healing. Indian J Plast Surg. 2012;45(2):316-324. doi:10.4103/0970-0358.101309
Chen HL, Cai J-Y, Du L, Shen H-W, Yu H-R, Song Y-P, Zha ML. Incidence of pressure injury in individuals with spinal cord injury. Journal of Wound, Ostomy and Continence Nursing: May/June 2020 – Volume 47 – Issue 3 – p 215-223 doi: 10.1097/WON.0000000000000633
Cowan LJ, Ahn H, Flores M, Yarrow J, Barks LS, Garvan C, Weaver MT, Stechmiller J. Pressure ulcer prevalence by level of paralysis in patients with spinal cord injury in long-term care. Advances in Skin & Wound Care: March 2019 – Volume 32 – Issue 3 – p 122-130 doi: 0.1097/01.ASW.0000553109.70752.bf
Delparte, J.J., Flett, H.M., Scovil, C.Y. et al. Development of the spinal cord injury pressure sore onset risk screening (SCI-PreSORS) instrument: a pressure injury risk decision tree for spinal cord injury rehabilitation. Spinal Cord (2020). https://doi.org/10.1038/s41393-020-0510-y
Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised National Pressure Ulcer Advisory Panel Pressure Injury staging system: Revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585-597. doi:10.1097/WON.0000000000000281
Fiordelli M, Zanini C, Amann J, Scheel-Sailer A, Brach M, Stucki G, Rubinelli S. Selecting evidence-based content for inclusion in self-management apps for pressure injuries in individuals with spinal cord injury: Participatory design study. JMIR Mhealth Uhealth 2020;8(5):e15818 DOI: 10.2196/15818 PMID: 32432559 PMCID: 7270844
Gour-Provencal G, Mac-Thiong J-M, Feldman DE, Bégin J, Richard-Denis A. Decreasing pressure injuries and acute care length of stay in patients with acute traumatic spinal cord injury. The Journal of Spinal Cord Medicine, 2020. DOI: 10.1080/10790268.2020.1718265
Grigorian A, Sugimoto M, Joe V, Schubl S, Lekawa M, Dolich M, Kuncir E, Barrios C, Nahmias J. Pressure ulcer in trauma patients: A higher spinal cord injury level leads to higher risk. J Am Coll Clin Wound Spec. 2017; 9(1-3): 24–31.e1. doi: 10.1016/j.jccw.2018.06.001 PMCID: PMC6304286 PMID: 30591898.
Harper AE, Terhorst L, Brienza D, Leland NE. (2020) Exploring the first pressure injury and characteristics of subsequent pressure injury accrual following spinal cord injury. The Journal of Spinal Cord Medicine, DOI: 10.1080/10790268.2020.1744871
Hogaboom NS, Worobey LA, Houlihan BV, Heinemann AW, Boninger ML. Wheelchair breakdowns are associated with pain, pressure injuries, rehospitalization, and self-perceived health in full-time wheelchair users with spinal cord injury. Archives of Physical Medicine and Rehabilitation Volume 99, Issue 10, October 2018, Pages 1949-1956. https://doi.org/10.1016/j.apmr.2018.04.002
Kloth, LC. Electrical stimulation for wound healing: A review of evidence from in vitro studies, animal experiments, and clinical trials. Sage Publications, 2005, LOWER EXTREMITY WOUNDS 4(1);2005 pp. 23–44, Sage Publications.
Kranke P, Bennett MH, Martyn-St James M, Schnabel A, Debus SE, Weibel S. Hyperbaric oxygen therapy for chronic wounds. Cochrane Database of Systematic Reviews 2015, Issue 6. Art. No.: CD004123. DOI: 10.1002/14651858.CD004123.pub4
Kruger EA, Pires M, Ngann Y, Sterling M, Rubayi S. Comprehensive management of pressure ulcers in spinal cord injury: current concepts and future trends. J Spinal Cord Med. 2013;36(6):572-585. doi:10.1179/2045772313Y.0000000093
Lemmer DP, Alvarado N, Henzel K, Richmond MA, McDaniel J, Graebert J, Schwartz K, Sun J, Bogie KM. What lies beneath: Why some pressure injuries may be unpreventable for individuals with spinal cord injury. Archives of Physical Medicine and Rehabilitation, Volume 100, Issue 6, June 2019, Pages 1042-1049. https://doi.org/10.1016/j.apmr.2018.11.006
Levine SM, Sinno S, Levine JP, Saadeh PB. An evidenced-based approach to the surgical management of pressure ulcers. Ann Plast Surg 2012;69:482–4. doi: 10.1097/SAP.0b013e31824b26bc.
National Center for Complementary and Integrated Health (NCCIH). Common skin conditions at a glance. https://www.nccih.nih.gov/health/skin-conditions-at-a-glance
Posthauer ME, Banks M, Dorner B, Schols J. The role of nutrition for pressure ulcer management. Advances in Skin & Wound Care: April 2015 – Volume 28 – Issue 4 – p 175-188 doi: 10.1097/01.ASW.0000461911.31139.62
Scheel-Sailer, A., Wyss, A., Boldt, C. et al. Prevalence, location, grade of pressure ulcers and association with specific patient characteristics in adult spinal cord injury patients during the hospital stay: a prospective cohort study. Spinal Cord 51, 828–833 (2013). https://doi.org/10.1038/sc.2013.91
Schwartz K, Henzel MK, Richmond MA, Zindle JK, Seton JM, Lemmer DP, Alvarado N, Bogie KM. (2020) Biomarkers for recurrent pressure injury risk in persons with spinal cord injury. The Journal of Spinal Cord Medicine, 43:5, 696-703, DOI: 10.1080/10790268.2019.1645406
Sherman RA, Wyle F, Vulpe M. Maggot therapy for treating pressure ulcers in spinal cord injury patients. The Journal of Spinal Cord Medicine, 18:2, 71-74, DOI: 10.1080/10790268.1995.11719382
Sun Y-S. Electrical stimulation for wound-healing: Simulation on the effect of electrode configurations. BioMed Research International, vol. 2017, Article ID 5289041, 9 pages, 2017. https://doi.org/10.1155/2017/5289041
Tasleem S, Naqvi SB, Khan SA, Hashimi K. ‘Honey ointment’: a natural remedy of skin wound infections. J Ayub Med Coll Abbottabad. 2011;23(2):26-31. PMID: 24800336
Thakral G, LaFontaine J, Najafi B, Talal TK, Kim P, Lavery LA. Electrical stimulation to accelerate wound healing. Diabet Foot Ankle. 2013; 4: 10.3402/dfa.v4i0.22081. doi: 10.3402/dfa.v4i0.22081. PMCID: PMC3776323. PMID: 24049559
Ud-Din S, Bayat A. Electrical stimulation and cutaneous wound healing: A review of clinical evidence. Healthcare (Basel). 2014 Dec; 2(4): 445–467. doi: 10.3390/healthcare2040445 PMCID: PMC4934569 PMID: 27429287
Vos-Draper TL, Morrow MMB. Seating-related pressure injury prevention in spinal cord injury: A review of compensatory technologies to improve in-seat movement behavior. Curr Phys Med Rehabil Rep. 2016;4(4):320-328. doi:10.1007/s40141-016-0140-7
Zanini, C., Lustenberger, N., Essig, S. et al. Outpatient and community care for preventing pressure injuries in spinal cord injury. A qualitative study of service users’ and providers’ experience. Spinal Cord 58, 882–891 (2020). https://doi.org/10.1038/s41393-020-0444-4