Poor Circulation in the Extremities
Join Our Movement
What started as an idea has become a national movement. With your support, we can influence policy and inspire lasting change.
Become an Advocate
You can assist with improving your blood flow by wearing compression stockings or gloves. These apply a slight tension to the skin which creates a very light compression internally making the inside of the body tighter. The resistance then improves blood flow. Elevating your legs and arms to reduce edema and facilitate return blood flow by using gravity is also helpful. Drink fluid, especially water, according to your catheterization needs, to increase overall blood volume. Check your medications to see if any of your prescriptions constrict blood flow. Keep chronic disease under control such as following a healthy diet and taking prescribed medications, especially if you are diabetic or have chronic heart disease. Provide movement to your extremities through range of motion exercises to activate your muscles for the pumping action to the blood vessels. If you have a genetic family history of poor circulation or other health problems that can lead to poor blood flow, attempt a preventative program to avoid or delay onset.
Massage is not recommended for stimulation of blood flow as it is not long lasting, increases constriction through pressure and can release an undiagnosed blood clot.
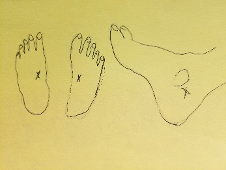
Poor circulation can become quite a serious problem. If poor blood flow develops, there are surgeries to re-route blood flow to the extremities. This is typically performed much later in vascular disease. Should the problem become such that re-routing blood flow does not help, amputation may be needed. Amputation is performed at the level where your circulation is still effective, not just at the site of the issue.
Some will suggest amputation early on especially if you have a spinal cord injury. Regardless of your SCI, amputation should only be done as a last resort. If someone does not want to offer another solution first, and there is still time for another option to work, it is appropriate to look for less radical medical treatments. If the limb can be saved, you do not have to have an amputation just because you have a spinal cord injury. Amputation may be necessary for your condition but not as an excuse.
As stated, poor circulation leading to vascular issues can be an issue in individuals with spinal cord injury. The risk factors are enhanced due to spinal cord injury. Being educated and aware can help you in noticing a problem that could be lurking in your health history. Nurse Linda
Pediatric Consideration: Children typically have great body function, healthier skin, better circulation, just better functioning body systems because they have not been exposed to the excesses of life. However, diseases that have been noted in the elderly are creeping down the chronology of humans. Problems relegated to the elderly are now in the pediatric population. Adding the issue of spinal cord injury, adds risks as well.
You can help your child maintain good health by providing a healthy environment and diet for your child and role modeling a healthy lifestyle yourself. Following care guidelines for healthy living with a spinal cord injury will maintain your child’s wellbeing.