Bladder Management
Anyone can be affected by bladder dysfunction. Common healthcare issues that are associated with bladder issues are enlarged prostate, hormonal changes in women, obesity, constipation, diabetes issues affecting cognition such as Alzheimer’s disease and other dementia, and neurological diseases and injury for example, spinal cord injury, multiple sclerosis and Parkinson’s disease. Lifestyle factors can affect bladder function such as smoking, inactivity, over consumption of alcohol and sugary drinks, or a protein-based diet. Urinary issues can result as a side effect of certain medications. At times, the reason for bladder dysfunction is unclear.
How the Urinary System Works
Removing waste from the body is an important step in maintaining health. The urinary system consists of organs that complete this process. Removal of liquid waste from the body is a major function but also the urinary system is responsible for regulation of blood volume, blood pressure, and the chemical components of the body.
Elimination of liquid waste from the body begins with the kidneys. These are two organs, one on each side of the body at the back and bottom of the ribcage. Kidneys are in constant motion filtering blood. It does not matter what you are doing, the kidneys are filtering blood. The kidneys do slow their work at night due to certain hormones like vasopressin (antidiuretic hormone, ADH), so you do not have to wake up at night to toilet if you do not have bladder dysfunction.
On a typical day, the kidneys filter about 1,700 milliliters or about seven cups of blood. The waste collected from blood by the kidneys becomes urine. The kidneys are controlled by the autonomic nervous system which is the part of the nervous system that causes the body to work automatically, or without your conscious control.
From each kidney is a long muscular tube, called a ureter, that extends to the bladder. The ureters transport urine from the kidneys to the bladder. They are designed to work with a one-way flow from a kidney to the bladder using peristalsis or muscular contractions. The ureters are also controlled by autonomic nervous system through the pelvic splanchnic nerves and from the inferior hypogastric plexus. However, the peristalsis action is from pacemaker cells within the ureter.
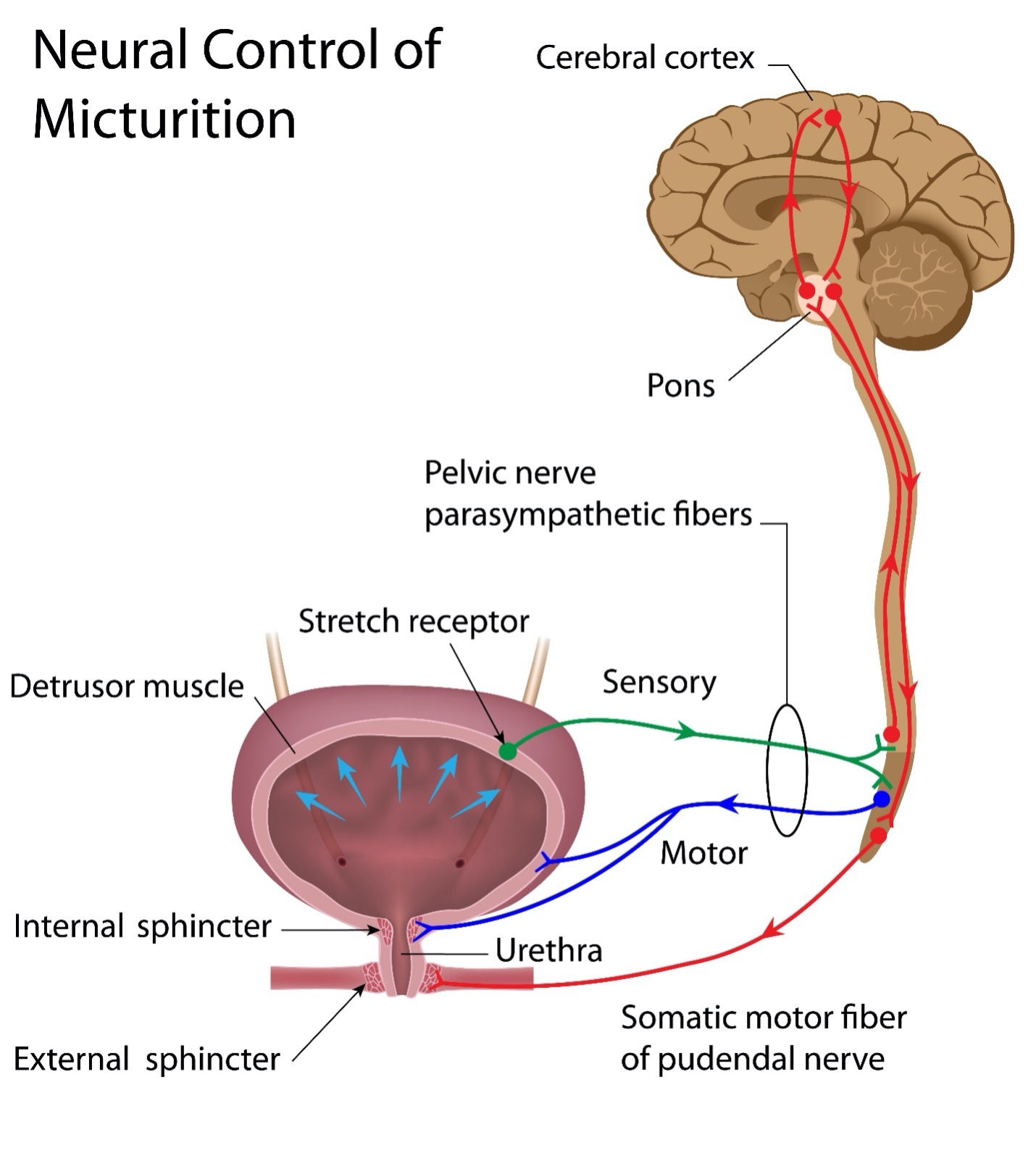
Once the urine enters the bladder, it is stored there until an appropriate time to release it. The bladder is a single organ at the bottom of the abdomen on the pelvic floor, just above the pubic bone. The bladder is medically called the detrusor muscle. The bladder will stretch as it fills with urine and contract as urine is emptied from it. As urine collects in the bladder, very slight contractions are triggered. These contractions become stronger as the bladder fills. The brain interprets the contractions to signal when it is time to empty the bladder.
Maximum capacity of the adult bladder is between 300-500ccs or 13 to 29 ounces. Overfilling of the bladder can lead to serious issues and consequences. Average amounts of urine in adults should be approximately two cups with slight variations in individuals. In children, bladder capacity is related to age but also affected by the child’s size. Estimation of pediatric bladder capacity is calculated using the formula: child’s age in years plus 2 and then multiple by 30. (AGE + 2)30 = pediatric bladder capacity in ccs. Alternatively, AGE + 2 provides the child’s bladder size in ounces.
The bladder consists of smooth muscle which is controlled by the autonomic nervous system, the sympathetic nerves of L2 and the parasympathetic nerves at S2,3,4. The sympathetic system regulates urine storage. The parasympathetic system controls bladder contractions and storage of urine. The pudendal nerve also exiting the spine at S2,3,4 also plays a part, especially in the external urinary sphincter.
The bladder has three openings, two at the top where the ureters enter to deliver urine from the kidneys and one at the base of the bladder for urine excretion. This opening for urine removal is called the urethra. The urethra is about eight inches long in males as it travels the length of the penis. In women, the urethra is about one and a half inches long.
The urethra contains two sphincters (circular muscles). The internal bladder sphincter is at the opening of the bladder. It is a part of the bladder muscle. It is under the control of the autonomic nervous system which means a person does not have voluntary control over it. When the bladder contractions are strong enough, urine will automatically flow out through the internal bladder sphincter. The second sphincter, the external sphincter is made of skeletal muscle which is under control of the somatic part of the nervous system. Somatic nerves are under your volitional control. You open and close the external sphincter muscle when you choose to empty urine from your bladder. The pudendal nerve also exiting the spine at S2,3,4 is the motor nerve for the external urinary sphincter.
In summary, the kidneys create urine, the ureters move the urine from the kidneys to the bladder, the bladder stores urine. When the urine is ready to be eliminated, the internal and external sphincters open, the bladder wall contracts, and urine is expelled. After urination is completed, the sphincters close so the bladder can again store urine. All of this must occur in precision and orderly coordination.
Please note for the following graphic that micturition is another word for urination.
What is Bladder Dysfunction
Issues of the bladder fundamentally appear in two ways, incontinence and retention. Urinary incontinence is an inability to control urine output until a socially acceptable moment. Urinary retention is an inability to empty the bladder either partially or fully. As nothing is simple in body function, a combination of retention and incontinence can occur. The source of urinary dysfunction leads to treatments.
Bladder dysfunction stems from a mismanagement by the body to regulate bladder contractions with sphincter function. This can be a result of many factors including illness and neurological issues. Bladder contractions that overpower the strength of the sphincters or weak sphincters can lead to urinary incontinence. Obstruction can lead to urinary retention. Issues with the central nervous system (CNS) causing miscommunication between the bladder and sphincters can lead to retention or neurogenic bladder.
There are several issues that can result from urinary system dysfunction.
Bladder atrophy is a small bladder that remains contracted. It is a result of not exercising the bladder with its stretch and contract ability. This most often occurs due to long term catheter placement either through the urethra or suprapubic opening which leads to immediate removal of urine rather than allowing bladder filling prior to emptying.
Bladder enlargement (hypertrophy) is thickened bladder muscle wall due to overstretching. Constantly over filling the bladder without emptying causes the muscles of the bladder wall to overstretch causing it to become thicker. The most common cause is obstruction but can be from neurological causes as well. A person with bladder hypertrophy has difficulty emptying the bladder and feels like they need to toilet often and has a slow stream.
Autonomic Dysreflexia (AD) Individuals with spinal cord injury, brain injury and those with medical diagnoses that affect the spinal cord can have disruptions in the autonomic nervous system (ANS). This is a miscommunication from the body below the level of spinal cord injury, usually at T6 or above. The body senses something is wrong but cannot identify the issue. Therefore, it triggers the ‘fight or flight’ response. Issues with the bladder are the primary source of AD. It is a medical emergency where the blood pressure becomes elevated 40 or more in systolic pressure (the top number) of the individual’s average blood pressure. The trigger needs to be found and removed.
Cancer of the Urinary System can develop in anyone. Risk factors include smoking (50% of bladder cancer is caused from smoking), exposure to toxic chemicals, some forms of radiation, and long-term infections. Previously, catheterization was a risk but is no longer since latex was removed from catheterization supplies.
Detrusor Sphincter Dyssynergia (DSD) occurs when the bladder muscle contractions do not work in harmony with the urethral sphincter. Either the bladder muscle will contract while the sphincter remains closed or the sphincter will open without successful bladder contractions for urine expulsion. A contracting bladder and closed sphincter can lead to reflux in the kidneys.
Infection of male anatomy Bacteria can spread from the urinary system to and from male organs as they share a communicating passage. This can include prostatitis, epididymitis and epididymo-orchitis (inflammation of the testis).
Kidney dysfunction and damage is caused when urine backs up in the urinary system, from infection and disease. The flow of urine is from the kidneys through the ureters to the bladder. However, backflow due to high pressure in the bladder or an obstruction that does not allow the natural passage of urine will cause urine to store in the kidneys where there is no capacity to do so. Diseases, such as diabetes and hypertension, also affect the ability of kidneys to function. Keeping the kidneys healthy is a priority in bladder management.
Obstruction can occur as a blockage in the kidneys, ureters, or urethra so that urine cannot pass through that part of the system. This can be from a stone, blood clot, stricture, scarring, enlarged prostate or other body organ or from fecal constipation or impaction.
Sepsis is an infection that travels throughout the body. It can begin in the urinary system or travel to the urinary system from another part of the body. Sepsis is a medical emergency. For more detailed information about sepsis: www.ChristopherReeve.org/cards
Stones are hard masses of crystals that mineralize to form stones. They can appear in any part of the urinary system. In the bladder, they may be small and pass without notice. Larger stones can impede the passage of urine and cause pain. Stones that pass through the ureters can be painful as the ureters are small in diameter. In the kidneys, there is no room for stones which can damage delicate tissues. The rough edges of stones can lead to bleeding. In those with spinal cord injury, stones can lead to episodes of autonomic dysreflexia and increased spasticity.
Urethritis is an inflammation or infection of the urethra (the opening in the body to the bladder.) This can occur for many reasons but, in individuals who catheterize, it can occur from leaving soap or cleaning solution on the urethra or surrounding area.
Urinary Reflux is the process of urine flowing backwards, up the ureters into the kidneys. As the kidneys have no capacity for storage, damage occurs which can lead to kidney failure.
Urinary Tract Infection is an infection anywhere in the urinary system. Most often, infections begin in the bladder which can then spread to the kidneys. It is critical to treat an infection as soon as possible to ensure it does not spread. Bacteria can enter the urinary system at any point. Most often, the entry is through the urethra where a large number of bacteria are typically found. Bacteria can invade any part of the urinary system. Treatment for infection should be promptly obtained.
Infections are easier to treat when caught early. Signs of a urinary tract infection are: persistent urge to urinate, burning especially with urination, frequent urination, cloudy, foul smelling, mucus, sediment or bloody urine, pain with urination or in the area of the pubic bone, lower back pain, fever, chills, nausea, headache, tiredness, spontaneous urine loss. Those with decreased sensation in the body may notice autonomic dysreflexia (AD) symptoms, increased spasticity, or referred pain to an area of the body where there is sensation especially the shoulder or jaw.
What Medications Have Urinary System Side Effects
Some drugs affect the urinary system. An excess or overdose of these medications, fluids and supplements can have side effects leading to a disruption in urinary functioning.
| Medication/ Fluid/Supplement | Effect on Urinary System |
| Alcohol | Urinary urgency, frequency, and functional incontinence. Decreased awareness of need to toilet. |
| Anticholinergics | Urinary retention and overflow incontinence. |
| Antidepressants | Urinary retention, overflow incontinence and dribbling. |
| Antipsychotics | Urinary retention, overflow incontinence and dribbling. |
| Antihypertensives | Stress incontinence especially in women |
| Caffeine | Urinary urgency, frequency, and incontinence. |
| Diuretics | Urinary urgency and frequency. Incontinence can be controlled by taking the medication early in the day and planned toileting. |
| Nonsteroidal anti-inflammatory drugs (NSAIDS) | Decreased awareness of need to toilet. Urgency, functional incontinence. |
| Opioids | Decreased awareness of need to toilet. Urgency, functional incontinence. |
| Sugary drinks | Urinary urgency and frequency. |
| Vitamin C, D | Frequent urination with overdosing |
Urinary Incontinence: Types and Treatments
Some individuals have urinary incontinence due to issues that do not arise necessarily from the central nervous system (CNS) or peripheral nervous system (PNS). The source of urinary system issues can also arise from hormonal changes, poorly toned muscles in the pelvic floor and diseases. Urinary incontinence should be discussed with your healthcare professional to ensure you are addressing and treating the correct issue. Those with spinal cord injury, some individuals with brain injury, and those with certain medical conditions have a neurogenic bladder which is miscommunication of the nerves. Continue below for more information about neurogenic bladder.
Urge Incontinence is a sudden urge to urinate with leakage of urine. This is from abnormal bladder contractions which can overpower the strength of the external sphincter to contain the urine in your body until an appropriate time to eliminate it.
The cause of urge incontinence is most often urinary tract infection but can be from disease such as diabetes, stroke, multiple sclerosis, Parkinson’s disease, bladder irritation or spinal cord damage. Any individual can develop urge incontinence, but it is most often found in the elderly, the obese, women with a history of C-section delivery or pelvic surgery, men with prostate conditions or surgery, or those with cancer of the bladder or prostate. Often the cause is unknown.
Treatment of urge incontinence involves changing behavior by toileting on a schedule which keeps your bladder empty to avoid triggering bladder contractions. Avoid caffeine, sugary drinks and alcohol which increase the urge to urinate. Avoid heavy lifting. Tighten the pelvic floor by performing Kegel exercises or using weighted vaginal inserts to strengthen pelvic muscles. Losing weight also helps reduce abdominal load. Biofeedback can be used to learn to reduce contraction responses.
Use of medications can reduce bladder contractions. There are many choices including: darifenacin (Enablex), fesoterodine (Toviaz), mirabegron (Myrbetriq), oxybutynin (Ditropan, Ditropan XL, Gelnique, Oxytrol), solifenacin (VESIcare), tolterodine (Detrol, Detrol LA), trospium (Sanctura), hyoscyamine (Anaspaz, Cystospaz, Hyosol, Hyospaz, Levbid, Levsin) or dicyclomine (Antispas, Bentyl, Byclomine, Di-Spaz, Dibent, Or-Tyl, Spasmoject).
Botox injections can be used in the bladder to reduce the frequency and severity of bladder contractions or spasms (tone). These injections will need to be repeated to maintain effectiveness.
Other treatments might include electrical stimulation to strengthen the urinary sphincters. There are also surgical techniques and implants that can increase sphincter compliance.
Overactive Bladder (OAB) is overactive bladder contractions that are often more continuous than episodic as in urge incontinence. Signs of OAB include the frequent urge to urinate and urinating more than 8-10 times during the day or two times at night. OAB may or may not be in addition to leakage of urine (urge incontinence). OAB and urge incontinence can be a mix of issues.
Overactive bladder can occur in anyone but can be a consequence of medical conditions such as multiple sclerosis, diabetes, hormonal changes during menopause, tumors, bladder stones, enlarged prostate, constipations, or as a result of surgery to treat other forms of urinary incontinence. Those with cognitive decline such as stroke, Alzheimer’s disease or other dementia are at risk for OAB. Urinary tract infections mimic the symptoms of OAB.
Behavioral changes can help OAB. These include urinating on a schedule. Practice holding or delaying urination for a short time eventually building to longer times. Changing fluids to decrease or eliminate caffeine, sugary drinks and alcohol will help decrease the urge to urinate. Tighten the pelvic floor with Kegel exercises and general body exercise. Maintain a healthy weight. Stop smoking to eliminate the bladder irritant nicotine. Biofeedback can be used to learn to reduce contraction responses.
In OAB, the bladder may not be able to be completely emptied when urinating. This triggers more contractions that are felt but not able to push out urine. If incomplete emptying of the bladder occurs, intermittent catheterization may be initiated.
If OAB is from hormonal changes in women, estrogen may be added to strengthen tissues. Medication may be used to help empty the bladder. These include tolterodine (Detrol), oxybutynin in pill form (Ditropan XL) or used as a skin patch (Oxytrol) or gel (Gelnique), trospium, solifenacin (VESIcare), darifenacin (Enablex), fesoterodine (Toviaz), or mirabegron (Myrbetriq).
Botox injections into the bladder can calm contractions. Electrical stimulation through the skin or as an implant in your body may be used to interrupt the bladder contraction signals. Surgery for more complicated OAB may be done such as bladder augmentation or enlargement or bladder removal.
Stress Incontinence is uncontrolled leakage of urine due to high intra-abdominal pressure. Typically, stress incontinence occurs with movement, heavy lifting, bending over, running, coughing, laughing, or sneezing. It is more common in women who have had multiple vaginal deliveries, hysterectomy or are post-menopausal. In men, it occurs more often after prostate surgery. Risk factors for both genders are aging, smoking or other medical issues resulting in heavy coughing, obesity, constipation, sexual intercourse and excessive caffeine and alcohol use.
Currently, there are no approved medications for treatment of stress incontinence. Estrogen may help reduce stress incontinence in women. The antidepressant drug duloxetine (Cymbalta) is being tested for treatment of stress incontinence with promising results. There are many over the counter products that are offered but outcomes vary.
Treatments for stress incontinence include pelvic floor exercises to strengthen muscles. Lifestyle changes of weight control, stopping smoking to reduce coughing, and curbing caffeine and alcohol intake are recommended. More advanced treatments are Botox injections, electrical stimulation, and surgically reconstructing the pelvic floor or gynecological surgery.
Overflow Incontinence results in dribbling of urine due to an inability to completely empty the bladder. The urge to empty the bladder is not felt. It is caused by an obstruction anywhere in the bladder outlet area from prostate issues or other narrowing or constriction of the urethra, a weak bladder muscle that cannot fully expel urine or nerve damage. The causes can be specific or a combination of issues.
Sources of overflow incontinence include temporary issues such as post-operative anesthesia or post-delivery. Diseases can lead to overflow incontinence including nerve damage from diabetes, alcoholism, Parkinson’s disease, multiple sclerosis, back problems/back surgery, or spina bifida. The side effects of some medications can lead to overactive bladder including certain anticonvulsants and antidepressants, that affect nerve signals to the bladder.
Treatment includes behavior changes such as scheduling bladder management and waiting 30 seconds after urinating and attempting to urinate again. Overflow incontinence can be treated with intermittent catheterization. Also, treating the underlying condition that is causing it will be necessary.
One medication for overflow incontinence is bethanechol, a cholinergic medication related to acetylcholine. It is available as Duvoid, Myotonachol, Urecholine, and Urocarb. For men, urinating with an enlarged prostate may be treated with alpha-adrenergic blockers such as doxazosin (Cardura), alfuzosin (Uroxatal), prazosin (Minipress), tamsulosin (Flomax), silodosin (Rapaflo), and terazosin (Hytrin).
Functional Incontinence is an issue where a person has recognition of the urge to urinate but simply cannot get to the toilet in time. The issue could be an inability to move their body fast enough, difficulty in removing their clothes, a physical impairment either in the body or from equipment or a thinking (cognitive) issue where the process is too complicated to work out.
Treatment for functional incontinence is to make the process easier through adjustments in clothing or physical surroundings. Toileting on a schedule can help as the urgency is reduced. If the source of the issue is a physical impairment that can be rectified, that should be a goal.
Mixed Incontinence is a combination of any of the above issues. A combination of the treatments may be required to address mixed incontinence.
What is Urinary Retention
Obstruction of the Urinary System occurs when something is blocking urine from fully or partially leaving the body. This occurs with enlarged prostate, constipation, bladder cancer, tumors, fibrosis, endometriosis, kidney stones and blood clots. It can be any issue that blocks any part of the urinary system from working or allowing urine to flow through the system or out of the body. Obstruction of the urinary system can occur pre-birth which is detected by blood tests of the mother and ultrasound.
Symptoms of obstruction include difficulty passing urine, slowed stream (dribble), frequency, decreased urine output, blood, or just feeling like your bladder is not empty.
Treatment is to remove or open the obstruction. If urine does not flow out of the body through the urethra, it will back up the ureters into the kidneys. Action must be taken quickly to prevent damage to the kidneys.
Treatment may include a temporary placement of an indwelling catheter, if possible, to open the urethra to allow urine to flow out. A stent may be placed in the ureter or urethra depending on the location of the blockage to open the flow. Surgery to correct the blockage issue is needed if the source of the blockage is an enlarged prostate, tumor or other obstruction.
Neurogenic Bladder (Neurogenic Bladder Dysfunction): Types and Treatments Neurogenic bladder occurs when there is an issue with the nerves and muscles that control bladder function. The parts of the urinary system need to work in coordination for effective urine elimination. Neurogenic means there is a difficulty with nerve transmission. When messages are impaired from being sent to and from the brain, a neurogenic bladder is diagnosed. This can be caused from disease or injury to the central nervous system (brain and spinal cord) or peripheral nervous system (nerves in the body). Examples of causes of neurogenic bladder include these and others:
- Medical issues affecting the brain or spinal cord
- Birth defects that effect the spinal cord
- Accidents to the brain or spinal cord
- Peripheral nerve damage
- Genetic nerve problems
- Infection in the urinary system or body
- Heavy metal poisoning
- Brain or spinal cord tumors
- Cerebral Vascular Accident (CVA) or stroke in
- the brain or spinal cord
- Diabetes
- Multiple Sclerosis
- Parkinson’s Disease
- Spina Bifida
- Cerebral Palsy
Types of neurogenic bladder are uninhibited, hyper-reflexive (spastic), flaccid and mixed.
Uninhibited neurogenic bladder is a reduced sensation or recognition that the bladder is full. Urinary incontinence (involuntary expelling of urine) occurs because the individual does not recognize the urge to void. It is associated with brain injuries, stroke, dementia, and multiple sclerosis.
An uninhibited neurogenic bladder may be treated by behavioral changes such as scheduling bladder management times with slowly stretching the time between voiding. Monitoring fluid intake and the type of fluids can avoid sudden accidents. Medications to tighten the sphincter muscles or relax bladder contractions (anticholinergics) may be used. Also, it may be necessary to begin an intermittent catheterization program (IMC) which is scheduled times of inserting a catheter to drain urine from the bladder.
Reflexive (hyper-reflexive) neurogenic bladder is typically found in individuals with injury to the upper motor neurons (UMNs) of the nervous system. Upper motor neurons (UMNs) are the primary source of movement in humans. The cell bodies of UMNs are in the upper part of the central nervous system, the brain and brainstem. UMNs connect to lower motor neurons (LMNs) through junctions called interneurons. Messages for movement follow this pathway unless disrupted by injury or disease. The results of UMN injury typically are seen in individuals with cervical and thoracic disease or injury. The reflexive neurogenic bladder occurs in individuals with spinal cord injury above T10.
When messages for movement are sent from the brain but the UMNs are damaged, the message is misinterpreted or not able to pass through. Damage to UMNs results in reflexive or spastic bladder. This might be seen outwardly in the body or have effects within the body.
One of the ways UMN injury is displayed is through a reflexive (spastic or tone) bladder. This bladder will fill with urine but will trigger an automatic emptying. The amount of urine expelled can be all the urine in the bladder or just a small amount. This is because the muscle of the bladder will contract as the sphincters do as well. This discoordination leads to urine being retained in the bladder creating high pressures which can cause urine to backflow up the ureters into the kidneys. As the kidneys do not store urine, damage is done. Treatments can prevent kidney damage.
Treatment for reflexive neurogenic bladder is approached depending on the individual’s needs. Men with higher level injuries where hand function is limited and have high pressure in the bladder may have a sphincterotomy performed. This is a surgical procedure where a small cut is made in the external sphincter muscle resulting in a free flow of urine out of the bladder. An external catheter is then used to collect and contain urine. This reduces the risk of urine flow back into the kidneys.
Due to women’s anatomy, a urine collection system is not available (although many are working towards one) so alternatives are used. For men or women, alternatives include suprapubic catheter, which is placed in a surgically created opening in the abdomen just above the pubic bone. A catheter is placed in this opening for free flow of urine. An alternative is use of an indwelling catheter through the urethra.
If hand function is sufficient, self-intermittent catheterization is initiated. This is a process where urine is drained from the bladder through a temporary catheter placement. Once the urine is drained, the catheter is removed. Fluids need to be monitored to avoid overfilling the bladder.
Flaccid neurogenic bladder The cell body of lower motor neurons (LMNs) are in the lower central nervous system in the spinal cord, nerve roots, cranial nerve nuclei of the brainstem and cranial nerves with motor function. LMNs receive messages from UMNs for movement. They connect directly with skeletal muscles for voluntary movement. Messages are sent from the brain to the body to move quickly, move slowly or stay as you are.
When the LMNs are damaged, messages from the brain are misinterpreted or not transmitted to the body. The result is flaccidity. LMN injury is most often seen in individuals with lumbar and sacral disease or injury. Nerves of the central nervous system (CNS) and possibly also the peripheral nervous system (PNS) are typically affected.
Below the level of injury, your body is also flaccid, including the bladder, which will fill with urine but not expel it. The bladder does not contract in the usual manner. Urine just continues to fill the bladder to overcapacity. At times, there might be an automatic expelling or incontinence of urine because the internal sphincter which is a part of the bladder muscle does not contract. Due to paralysis, the individual may not have voluntary control of the external urinary sphincter. Typically, the full amount of urine in the bladder is not eliminated. Residual urine remains in the bladder. It is possible that the bladder can become so full that it ruptures, or the person becomes incontinent (involuntary expelling of urine).
If the reflex arcs are preserved, stretching the rectal opening may result in expulsion of urine. This must be done on a timed basis as sensation signals of a full bladder are not received by the brain. Tapping over the area of the bladder can also stimulate urination for some. Treatment of flaccid neurogenic bladder can also be managed with intermittent catheterization.
Individuals with flaccid neurogenic bladder may be using Credé’s maneuver (rolling the hand down the skin over the bladder) or Valsalva maneuver (bearing down) as triggers for urination. To utilize these methods of voiding, you must ensure that you have low sphincter resistance so urine can easily flow out of the urethra. If your sphincter is tight, these activities build pressure in the bladder which can cause urine to back up into the kidneys. Although some still use Valsalva, it has been discontinued due to pressure in the rectum leading to prolapse. Check with your healthcare professional to ensure these practices are safe for your individual needs. If you have a tight sphincter, medication can be used to help relax it. Alternatively, a sphincterotomy, a small surgical cut in the sphincter muscle, may be done, however, this results in continuous urinary incontinence.
Mixed neurogenic bladder There are cases where individuals have elements of both the UMN and LMN injury. For example, the bladder can be reflexive, but the external sphincter is flaccid which leads to urinary incontinence. Or the bladder can be flaccid with a reflexive external sphincter. This creates a large, high pressure bladder with an inability to urinate.
Diagnosing Bladder Issues
Issues with bladder management should be diagnosed by healthcare professionals. Assuming that you have one type of bladder issue when it is another can lead to further complications and urinary system damage. Self-management can lead to serious complications especially to the kidneys. For example, treating what you think is overflow incontinence when you really have leakage from a neurogenic bladder can lead to high pressure in the bladder causing urine to back up into the kidneys. Testing is needed to determine the diagnosis followed by the correct treatment for a healthy urinary system for a lifetime.
Laboratory Tests
Blood Tests are performed by assessing a small sample of your blood. This can provide information about how your bladder and kidneys are functioning or if you have an infection in your body. Blood Urea Nitrogen (BUN), creatinine levels and Glomerular Filtration Rate (GFR) are some of the blood tests that are indications of kidney function. An increased white blood cell count indicates there is an infection somewhere in the body including the urinary system. Also, a blood test can indicate if you have enough hydration in your body to keep the urinary system functioning well. Men with suspected prostate enlargement may have a prostate-specific antigen (PSA) test and testosterone levels assessed.
Urinalysis and Culture and Sensitivity (UA & CS) Testing of urine can be performed to assess health indicators including urinary tract infections (UTIs), kidney disease, and diabetes among other issues. The urinalysis assesses acidity (pH), concentration or specific gravity, protein, sugar (glucose), ketones, bilirubin, signs of infection, and blood. Urine quality tests are amount of white blood cells, red blood cells, bacteria and yeast, casts (tube shaped proteins), and crystals.
If an infection is determined to be in the urine as indicated by the UA, a C&S is done using the same urine sample. The bacteria in the urine is allowed to grow in a culture dish. This is the culture part of the test. Then different antibiotics are evaluated to see which will eliminate the specific bacteria. This is the sensitivity part of the test. This process takes three days to complete. If you have an infection, the best choice of antibiotic is prescribed. You must take the entire prescription of the antibiotic to eliminate the bacteria. Even if you feel like the infection is gone, it is actually just getting under control. The infection is not eliminated until the entire prescription is taken.
24 Hour Urine Collection A collection of urine for one full day may be done to check kidney function. The objective is to see the amount of creatinine that is cleared by your kidneys. This test also assesses protein, urinary hormones, minerals, and other chemicals.
Clinical Testing
Post Void Residual (PVR) The post void residual is a method to assess if urine is left in the bladder after a spontaneous void or incontinence. In this procedure, the individual attempts to void or has a spontaneous or incontinent urine output. A straight catheter is inserted, any urine left in the bladder is drained and the catheter is immediately removed. The goal is to have no urine left in the bladder.
Bladder Scan One of the simplest assessments of bladder emptying is a noninvasive bladder scan. It is an ultrasound device that is placed on the skin over the bladder area. A transmission gel is placed on the device and skin to project sound waves into the bladder. A diagram of the urine in the bladder can be seen on a monitor with a measure of the amount of urine in the bladder. This procedure can replace the post void residual if the equipment is available. It is typically preformed in the acute care hospital, rehabilitation hospital or healthcare provider’s office.
Abdominal/Renal Ultrasound Testing An ultrasound assessment of the entire urinary tract can be performed in a testing center. The assessment includes the kidneys, ureters, and bladder (KUB). The examination provides a picture of the structures of the urinary system and can indicate the presence of stone or strictures.
Urodynamic Testing is the most important test of the urinary system for individuals with brain injury, spinal cord injury or other neurological issues especially of the central nervous system (CNS). This is an assessment of how the urinary system is functioning.
In urodynamic testing a sterile, pressure sensitive catheter is placed in the bladder. This catheter measures pressure in the abdomen, bladder, and urethra. A sensor is placed in the rectum to measure rectal pressure and a sensor is placed on the abdomen also to measure abdominal pressure. Fluoroscopic images may be taken during the procedure. Sterile fluid is slowly dripped into the bladder. As the bladder fills, pressures are measured. You will be asked if you feel any sensations and might be asked to try to empty your bladder–even if this is not your typical ability, it is requested to gather information.
Results will indicate your risk for reflux of urine into the kidneys which can damage them. The type of bladder function is identified, high or low pressure, hyperactive or flaccid. Nerve and muscle function are assessed. How the bladder and sphincters contract, if they coordinate, and their competence is analyzed. Depending on the results, treatments can be provided that will improve your urinary system and safety. Combinations of these procedures might be recommended.
Intravenous Pyelogram/Urogram In this test, a dye is injected into your body. While it passes through your body, radiology is performed to assess how well your urinary system is functioning. The dye is excreted quickly with your urine. The test evaluates the kidneys, ureters, bladder, and urethra. Issues such as kidney stones, tumors, cysts, narrowing of ureters and enlarged prostate can be identified.
Cystoscopy is a procedure where a narrow viewing tube is placed through the urethra into the bladder. This procedure is most likely performed under anesthesia. The inside of the bladder is then viewed by the examiner. The cystoscopy is used to look for infection, sources of bleeding, stones, inflammation, cancer or to remove small tumors. It can also help with diagnosis of an enlarged prostate. Samples of tissue can be inspected in your body or removed for laboratory review.
Bladder Biopsy During the cystoscopy, a biopsy of tissue that appears to be concerning can be done. The suspected tissue is then studied in the laboratory. This is especially important for identification of polyps or other growths.
Bladder Management
Bladder programs are developed for the urinary health of individuals with nerve damage. Neurogenic bladder is not an issue of re-learning urination but an issue of nerve miscommunication and gaining healthful, appropriate control of your bladder.
Bladder programs should not be confused with potty training. Babies are born without fully functioning muscles and nerves. It takes a while for the pelvic floor muscles to develop leading to bladder stabilization and for the nerves to develop to control urine output. When the bladder of a baby fills a message is sent to the brain to relax the sphincters. This happens automatically. As a child becomes older, they learn to suppress the automatic opening of the sphincter for self-control over urination. Older children and adults have accomplished nerve control of the external sphincter. Bladder programs are put into place because of an issue with the nerves of the body.
Procedures that gain control over bladder function include:
Bladder Augmentation is a process in which the bladder is surgically enlarged so it can contain a greater capacity of urine. This is not a urine removal process, but it allows larger capacities to be held within the bladder.
Electrical Stimulation Implant with Posterior Sacral Rhizotomy The nerves that control urination are S2 -S4. Implantation of an electrical stimulation device on the nerve roots can assist with sphincter and bladder contraction and relaxation. The electrodes are surgically attached to the nerve roots, not the spinal cord nerve itself. A rhizotomy is performed in which the selective reduction of nerve fibers that are creating too much tone affecting bladder and sphincter function are identified and cut or cauterized. These two procedures are performed in one surgery.
External Catheters for Men are used for men who have spontaneous elimination of urine from contraction, overflow of the bladder or incompetent sphincters. External catheters are sometimes called condom catheters because of their resemblance to condoms. They consist of a sheath secured around the outside of the penis that has an opening at the end to collect urine as it is spontaneously released from the bladder. The open end is connected to a leg bag or night drainage bag either with a tubing extension or directly.
External catheters are used as the bladder management system for men whose bladders spontaneously release the entire contents of urine collected in the bladder or, more likely, in conjunction with a sphincterotomy that allows urine to flow freely. External catheters are used as a collecting device for breakthrough urination between intermittent bladder catheterizations. If all urine is not spontaneously emptied from the bladder, a combination of external catheter and intermittent catheterization is used.
Sometimes, the pressure of urine output is greater than the drainage opening of the external catheter. This can cause the external catheter to blow up like a balloon until the urine drains. You will need to keep the external catheter clear from constrictions like between the legs to allow this to happen. Sometimes, the catheter will explode due to the force of urine output. Avoid using excessive tape to secure the catheter as this can lead to damage to the penis. If this happens regularly, try a different brand or size of external catheter.
External Catheters for Women As the female anatomy is internal, it has been difficult to develop a device for external catheter placement. Through the years, there have been many attempts from unsuccessful apparatuses to even surgical rearrangement of the anatomy to meet women’s needs with urinary incontinence from any cause including high pressure bladders.
New devices are on the market. Seeing the need to control female urinary incontinence from non-nerve issues, there are a few new options that are now available. As these devices are new, the idea of use along with a sphincterotomy for women may be a way for the future. The new devices are unproven in neurogenic bladder as they collect expelled urine and don’t remove urine from the bladder.
These devices fit within or surrounding the labia. They pull expelled urine away from the body. Some have a flange that fits in the labia around the urethral opening. This helps overflow or leakage but will not empty a neurogenic bladder. Intermittent catheterization still needs to occur.
The important point is that incontinence in women with spinal cord injury is being addressed. This will reduce the dependence on adult incontinence pads that have skin breakdown issues and indwelling catheters.
Indwelling urethral catheters are mostly used long-term by women with high pressure bladder, an inability to perform intermittent catheterization, or due to lack of external catheter options. Men occasionally use indwelling urethral catheters but less often. The indwelling catheter allows a continuous flow of urine while keeping the urine contained and skin dry which avoids pressure injury. The indwelling catheter is connected to a leg bag or night collection bag. Connecting tubing may or may not be used.
The indwelling catheter should be secured using paper tape to the thigh or a catheter thigh strap for a woman to keep it from pulling with movement. For men, paper taping the indwelling catheter tubing up onto the abdomen allows a more direct flow of urine out of the bladder.
Indwelling catheters should be changed using sterile technique on a schedule indicated by your healthcare professional. The area at the urethra should be cleaned as per instructions of the healthcare professional. Over time, an indwelling catheter will dilate the urethra. If urine leaks around the indwelling catheter, a larger size or larger balloon is needed.
Individuals with indwelling catheters can drink fluids freely unless restricted by other medical conditions. Keeping urine flowing out of the body is one of the best ways to avoid urinary tract infections.
Cleaning the connections with alcohol each time the system is opened and keeping the drainage bag lower than the level of the bladder are other ways to avoid bacteria from entering the bladder. When in bed or seated, be sure the drainage bag is hooked onto the side of the bed, chair or your leg, lower than the bladder and that the drainage tube is coiled on the bed next to you. Dependent drainage tubes do not let urine flow freely out of the bladder. The drainage bag should never be placed on the floor.
Intermittent Catheterization (IMC) is the most preferred method of bladder management because it mimics the natural stretching and contracting of the bladder muscle and has less risk of infection. The system can be used by individuals with high- or low-pressure bladders, reflexive or flaccid bladders. This is the basic IMC process:
| Step | Process | Why |
| 1 | Collect your equipment, catheter, lubricant, urethral cleaning supply | -Once you begin, you do not want to interrupt your procedure. If you do, you will need to wash your hands again and could contaminate your supplies.-Keep supplies together and handy. |
| 2 | Get into position for catheterizing. This can be on the toilet, next to the toilet, in your chair, in bed | -Sitting takes advantage of gravity to empty the bladder.-Being on the toilet makes an easy clean up as you can simply flush the urine away.-If you must catheterize in bed, be sure to sit up, if possible. |
| 3 | Wash your hands | -Use warm, flowing water and soap, rubbing vigorously for 20 seconds or two rounds of happy birthday.-Dry with a clean towel. Used towels collect bacteria so use a clean one when possible.-Once your hands are clean, you do not want to dirty them when moving yourself to your cathing location. |
| 4 | Open supplies | -At home, supplies are ordered separately for your needs.-There will be several different items to open.-Once open, keep supplies on the inside of the packaging to maintain cleanliness. |
| 5 | Drop lubricant onto catheter | -If the lubricant tube opening touches anything, including your catheter, it is no longer clean. Drop the lubricant from the tube to the catheter without touching the opening of the tube.-Lubricate the catheter for the length of insertion. Men 6-8 inches, women 2 inches.-A well lubricated catheter lessens damage to the urethra and passes much more smoothly. |
| 6 | Clean the opening to the bladder | -Most people will use soap and water.-Use a gentle soap to avoid irritation of the urethra.-Wash from front to back of the urethra in one swipe. Then remove the washcloth from your skin. Wash front to back again. Repeat this process. This avoids recontamination of the urethra.
-Scrubbing back and forth can irritate the urethra and leads to recontamination. |
| 7 | Insert well lubricated catheter until urine starts flowing out | -The catheter is in far enough when urine starts to flow out. |
| 8 | Drain urine until it stops flowing | – Once urine stops flowing, the level of the urine is below the eye of the catheter. That does not mean your bladder is empty. |
| 9 | Slowly remove catheter | – Slow removal will drain that last bit of urine left in the lowest part of your bladder. |
| 10 | Clean residue from bladder opening | -Leaving soap or urethra cleaning solutions can dry and crack skin providing opportunity for bacteria to enter. |
| 11 | Clean up and discard supplies | – Clean the area where you catheterized by picking up your equipment and disposing of it properly. |
| 12 | Wash your hands | -Always thoroughly wash your hands after voiding. |
Intermittent catheterization is done every four to six hours. Your timing schedule will be established by your healthcare provider as based on your needs. It is critical that you maintain your schedule to avoid overfilling your bladder resulting in possible incontinence or backflow into the kidneys.
Fluids need to be monitored with IMC. Men should have about 350ccs, women about 300ccs of urine in their bladder at catheterization time to avoid overstretching and back flow. Some fluids such as sugary drinks, caffeine, or alcohol pass through the body quicker than water so you can easily overfill your bladder with these drinks. You can still enjoy them, just use moderation. However, plain water is best.
Advantages to IMC include keeping the bladder exercised as the natural stretching and contracting of the bladder wall is maintained. There are less urinary tract infections with this procedure as the catheter is not left in the bladder.
Mitrofanoff Procedure A surgical procedure where an opening is created in the navel (belly button) with use of repurposing the appendix or part of the bowel to create a new pathway to the bladder. A straight catheter is used to remove urine. Then the catheter is removed. This procedure was developed for children but adults with SCI find it helpful especially for women as access is practical. Some men opt for this in unique situations such as retracted penis. The catheterization, timing and fluids process is much like intermittent catheterization.
Ostomy A surgical procedure creating an opening in the abdomen which allows the output of urine to flow into a collection bag worn on the abdomen. The ostomy area must be cleaned carefully as the opening is directly into the urinary system. Fluids are typically freely consumed as the urine is constantly flowing out of the body.
Reflex Bladder Emptying Individuals with lower level spinal cord injury in the lumbar or sacral levels of the spine will find that they may expel some urine when performing their bowel program. This can be harnessed to empty the bladder by stretching the rectum. Use of tapping over the bladder can stimulate a spontaneous expulsion of urine. Credé is a technique where one rolls their fingers over the bladder on the skin of the abdomen from top to bottom. Valsalva or bearing down is less often recommended due to complications such as rectal prolapse. It is bearing down to create pressure in the abdomen to push out urine. Reflex techniques need to be approved by your healthcare professional or urologist as the added pressure can cause reflux of urine into the kidneys and prolapse of the rectum.
Sphincterotomy is a small incision in the external urinary sphincter to allow for free release of urine. Both the internal and external urinary sphincters typically will open with bladder contractions. If there is an issue in the process, one or both sphincters will be surgically opened by a small slit. The procedure is typically performed under anesthesia or sedation by inserting a tube through the urethra or bladder opening. The incision(s) are then made through the access of this tube. It is typically done early after a traumatic spinal cord injury but can be done at any time when needed if a disease progresses affecting bladder function.
This procedure is performed in men who have high pressure or the risk of developing high pressure bladders from overactive bladders or detrusor-sphincter dyssynergia (DSD where the sphincters do not work in conjunction with bladder contractions. With spinal cord injury, this procedure is more often done in men because an external catheter can be used to collect and contain the urine flow.
There are typically no restrictions of fluid after this procedure. Fluid is encouraged unless restricted by other healthcare issues. Intake of fluid helps flush the urinary system of toxins and bacteria as well as maintaining general health.
Suprapubic Catheter is used for individuals who have high pressure bladders or are at extreme risk for high bladder pressure. It is usually done early after trauma but can be recommended anytime in disease processes or with the development of uncontrolled or increased pressures in the bladder.
Suprapubic catheters are placed through a surgical opening in the skin above the pubic bone over the bladder. A catheter is then placed through this opening for continuous drainage of urine. Eventually, the skin will heal around the edges of the opening but will remain open around the catheter.
The catheter is changed using sterile technique. Changing the catheter is dependent on your needs, typically every month to ten weeks but sometimes as often as every other week or more frequently. A sterile dressing is placed around the catheter at the opening in the skin to protect the wound. The wound area needs cleaning and the dressing should be changed one to two times per day. The catheter drains into a drainage bag or leg bag. The tubing from the catheter to the drainage collection system should be secured to the abdomen or upper thigh to keep from pulling the catheter or dislodging it during dressing, transfers or activity. With proper care, infection rates are about the same as intermittent catheterization.
Urethral Stents are small structures to open the urethra. These are helpful to those with detrusor sphincter dyssynergia (DSD) or individuals who use reflex techniques for urinating.
Urinary Diversion, Continent Urinary Diversion, Cutaneous Ileovesicostomy are procedures where the ureters are connected to a part of the bowel which is then opened to the abdomen. A bag collects urine as it is produced. The bladder may remain or be removed depending on the needs of the individual. It is done when other options or complications of the urinary system require it.
Medications for Neurogenic Bladder
There are an extremely large number of individual drugs that are available for treatment of specific issues with neurogenic bladder. Categories of drugs and their purpose are listed here.
Anticholinergic Medications work by blocking cholinergic transmission at muscarinic receptors. These drugs decrease bladder contractions and spasms to reduce and eliminate overflow incontinence. Side effects are drowsiness, blurred vision, heart palpitations and facial redness, among others.
Antidepressants relax the bladder muscle. Typically, tricyclics are used. If you use an antidepressant for treatment of mental wellness, you can benefit from the side effect of bladder muscle relaxation.
Antispasmodics relax the bladder muscle so more urine can be held prior to elimination. Side effects include interference with activities that require physical coordination and mental alertness
α-blockers (alpha-blockers) treat detrusor sphincter dyssynergia (DSD) and low bladder pressure. They should not be taken by those with extremely low blood pressure or orthostatic hypotension.
Botulinum Toxin Injections are used as a treatment directly into the urinary sphincter and/or bladder for detrusor sphincter dyssynergia (DSD). The medication relaxes contraction. Repeated treatments are required to continue effectiveness.
Types of Catheters
Catheters come in a variety of types and sizes. Adults will generally begin with a size 12Fr (catheters are measured in sizes called French). Children will have much smaller sizes. If catheters are left in place in the body, dilation of the urethra or suprapubic opening can occur. This may require the next size catheter to avoid leaking.
Indwelling Catheters are left in the body. Typically, these are used in the urethral opening or suprapubic site. They are held in place by a balloon which is sized by the amount of fluid used to inflate the balloon. These catheters come in an insertion kit and will have a drainage bag included. A daytime, more discrete leg bag can be substituted.
Intermittent Catheters are used to empty urine and then removed. They may be one time use or you may receive instructions for sterilizing the catheter between uses. The most common type is the non-coated straight catheter. These catheters require you to use a water-soluble lubricant for insertion. Basic catheters are typically funded by your payor source (health insurer). Specialty catheters that require special payor authorization include hydrophilic coated catheters which have a polymer solution that lubricates the catheter for smooth insertion. Closed intermittent catheters are encased in a urine collection bag so you do not touch the catheter. They are coated with gel, hydrophilic, or antibacterial substances.
Female Catheters are shorter versions of the standard intermittent catheters, generally 7-9 inches in length. They are convenient for intermittent catheterization that are more in proportion to the female anatomy.
Labia Separators are devices that can help position women for catheterization. The device frees up both hands for catheterization. Use of both hands allows you to balance better.
Coudé Catheters have a curved tip at the insertion. These are used if there is an obstruction such as enlarged prostate. The curved tip can slide around the obstruction.
Bladder Management Professional Team
Those who may be involved with your bladder management program include:
A Physiatrist is a physician who specializes in rehabilitation who will diagnose neurogenic bladder or other bladder issues. They determine the type of bladder management needed, provide necessary medications, and follow your progress through the years.
A Urologist is a physician who specializes in the urinary system. Testing, procedures, and surgery of the urinary system are conducted by this specialty.
The Rehabilitation Registered Nurse will be key in teaching you to perform catheterization and other bladder management techniques. The registered nurse can help with reducing complications and problem solving.
A Physical Therapist will help with balance, strengthening exercises for the body and with the pelvic floor muscles. They will assist in learning to transfer for toileting.
An Occupational Therapist works with fine motor control to teach you how to hold catheters as well as use of adaptive equipment.
An Insurance Case Manager will be key should you need an advanced catheter or specialized equipment to improve your function and independence.
The Psychologist is an important member of the team in helping you strengthen your mental wellness in case issues with your bladder management become overwhelming.
Bladder Management Research
There has been extensive research of bladder management. Medications and developments in catheters have advanced over the last 10-20 years with more innovations continuing. However, issues for bladder management still abound. A perfect system has yet to be identified. Every aspect of bladder management is under research, from diagnosis to treatment to medications, even education.
The mechanism of bladder management for incontinence and retention issues are being examined by researchers. Specifically, why individuals develop urinary incontinence is being studied. Factors include hormonal changes, aging, obstruction, infection, and neurogenic issues. Understanding why and how the urinary system works within itself as well as with other systems of the body leads to being able to alter outcomes.
Neurogenic bladder and treatments are included in the study of the brain and spinal cord. New treatments include stem cell and tissue engineering initiatives that would create functional abilities for individuals with bladder management issues. Other procedures are being tested to further understand the intricacies of urodynamic testing. Surgical improvements are also being researched including both anatomic alteration and electrical stimulation to return function.
Catheter development has exploded over the past two decades. They have become more body friendly as well as user friendly. Research supporting the efficacy of use is critical to increasing the payment method system for global funding.
One of the most critical areas of study is education of individuals to understand the details of bladder management. Knowing what is critical to successful urinary health can increase quality of life.
Bladder Management Facts and Figures
In all populations:
Urinary incontinence is reported in about 3% to 17% of women. Severe incontinence noticeably increases at age 70-80 mostly caused by hormonal changes.
Urinary incontinence in reported in about 3% to 11% of men. Of men with urinary incontinence, urge incontinence is noted at 40% to 80%. Stress incontinence is less than 10% of cases and is attributable to prostate surgery, trauma, or neurological injury.
In individuals with spinal cord injury:
The number of individuals with neurogenic bladder varies by disease. This is because diseases are reported but outcomes such as neurogenic bladder is not. Therefore, a variety of estimates are reported depending on the study.
Spinal cord injury from trauma or disease 70-84%
Multiple Sclerosis 40-90%
Parkinson’s Disease 37-72%
Stroke 15%
An average of 2.5 urinary tract infections per year are reported by those with SCI.
Resources
If you are looking for more information about bladder management or have a specific paralysis-related question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm EST.
Additionally, the Reeve Foundation maintains fact sheets with additional resources from trusted Reeve Foundation sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to paralysis-related organizations, including associations which features news, research support, and resources, national network of support groups, clinics, and specialty hospitals.
Community Resources:
American Cancer Society: Treatment of Bladder Cancer by Stage https://www.cancer.org/cancer/bladder-cancer/treating/by-stage.html
Cleveland Clinic: Neurogenic Bladder https://my.clevelandclinic.org/health/diseases/15133-neurogenic-bladder
Craig Hospital: Bladder Management Tools for Men with Spinal Cord Injuries https://craighospital.org/resources/bladder-management-tools-for-men-with-spinal-cord-injuries
Johns Hopkins: Neurogenic Bladder https://www.hopkinsmedicine.org/health/conditions-and-diseases/neurogenic-bladder
Kessler Foundation: Comparing Drug Treatments for Neurogenic Detrusor Overactivity in SCI https://kesslerfoundation.org/research/studies/comparing-drug-treatments-neurogenic-detrusor-overactivity-sci
Northwest Regional Spinal Cord Injury System: SCI Empowerment Project Health Guides: Bladder http://sci.washington.edu/empowerment/health_guides.asp
Shepherd Center: Bladder Care https://www.myshepherdconnection.org/sci/bladder-care
Shirley Ryan Abilities Laboratory: Understanding Neurogenic Bladder, https://www.sralab.org/lifecenter/resources/understanding-neurogenic-bladder-download
Clinical Practice Guidelines:
American Urological Association: Diagnosis and Treatment of Non-Neurogenic Overactive Bladder (OAB) in Adults: an AUA/SUFU Guideline (2019) https://www.auanet.org/guidelines/overactive-bladder-(oab)-guideline
American Urological Association: Clinical Guidelines https://www.auanet.org/guidelines?q=,&ContentType=Best_Practice_Statements,Best_Practice_Statements&filters=,790%7C
Centers for Disease Control and Prevention (CDC): Community-Associated Urinary Tract Infection (CAUTI) Treatment Guidelines https://www.cdc.gov/infectioncontrol/guidelines/cauti/index.html
Paralyzed Veterans of America: Bladder Management for Adults with Spinal Cord Injury: Clinical Practice Guidelines for Healthcare Professionals https://www.pva.org
References
Abolhasanpour N, Hajebrahimi S, Ebrahimi-Kalan A, Mehdipour A, Salehi-Pourmehr H. Urodynamic parameters in spinal cord injury-induced neurogenic bladder rats after stem cell transplantation: A narrative review. Iran J Med Sci. 2020 Jan;45(1):2-15. doi: 10.30476/ijms.2019.45318. PMID: 32038054; PMCID: PMC6983271.
Adriaansen JJ, van Asbeck FW, Tepper M, Faber WX, Visser-Meily JM, de Kort LM, Post MW. Bladder-emptying methods, neurogenic lower urinary tract dysfunction and impact on quality of life in people with long-term spinal cord injury. J Spinal Cord Med. 2017 Jan;40(1):43-53. doi: 10.1179/2045772315Y.0000000056. Epub 2016 Apr 8. PMID: 26446581; PMCID: PMC5376129.
Cooper FP, Alexander CE, Sinha S, Omar MI. Policies for replacing long-term indwelling urinary catheters in adults. Cochrane Database Syst Rev. 2016 Jul 26;7(7):CD011115. doi: 10.1002/14651858.CD011115.pub2. PMID: 27457774; PMCID: PMC6457973.
Ginsberg D. The epidemiology and pathophysiology of neurogenic bladder. Am J Manag Care. 2013;19(10 Suppl):s191-6. PMID: 24495240.
Hachem LD, Ahuja CS, Fehlings MG. Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J Spinal Cord Med. 2017 Nov;40(6):665-675. doi: 10.1080/10790268.2017.1329076. Epub 2017 Jun 1. PMID: 28571527; PMCID: PMC5778930.
Haglind E, Carlsson S, Stranne J, Wallerstedt A, Wilderäng U, Thorsteinsdottir T, Lagerkvist M, Damber JE, Bjartell A, Hugosson J, Wiklund P, Steineck G; LAPPRO steering committee. Urinary incontinence and erectile dysfunction after robotic versus open radical prostatectomy: A prospective, controlled, nonrandomised trial. Eur Urol. 2015 Aug;68(2):216-25. doi: 10.1016/j.eururo.2015.02.029. Epub 2015 Mar 12. PMID: 25770484.
Hamid R, Averbeck MA, Chiang H, Garcia A, Al Mousa RT, Oh SJ, Patel A, Plata M, Del Popolo G. Epidemiology and pathophysiology of neurogenic bladder after spinal cord injury. World J Urol. 2018 Oct;36(10):1517-1527. doi: 10.1007/s00345-018-2301-z. Epub 2018 May 11. PMID: 29752515.
Han CS, Kim S, Radadia KD, Zhao PT, Elsamra SE, Olweny EO, Weiss RE. Comparison of urinary tract infection rates associated with transurethral catheterization, suprapubic tube and clean intermittent catheterization in the postoperative setting: A network meta-analysis. J Urol. 2017 Dec;198(6):1353-1358. doi: 10.1016/j.juro.2017.07.069. Epub 2017 Jul 20. PMID: 28736320.
Hu HZ, Granger N, Jeffery ND. Pathophysiology, Clinical importance, and management of neurogenic lower urinary tract dysfunction caused by suprasacral spinal cord injury. J Vet Intern Med. 2016 Sep;30(5):1575-1588. doi: 10.1111/jvim.14557. Epub 2016 Aug 16. PMID: 27527382; PMCID: PMC5032886.
Feneley RC, Hopley IB, Wells PN. Urinary catheters: history, current status, adverse events and research agenda. J Med Eng Technol. 2015;39(8):459-70. doi: 10.3109/03091902.2015.1085600. Epub 2015 Sep 18. Erratum in: J Med Eng Technol. 2016;40(2):59. PMID: 26383168; PMCID: PMC4673556.
Maserejian NN, Giovannucci EL, McVary KT, McKinlay JB. Intakes of vitamins and minerals in relation to urinary incontinence, voiding, and storage symptoms in women: a cross-sectional analysis from the Boston Area Community Health survey. Eur Urol. 2011 Jun;59(6):1039-47. doi: 10.1016/j.eururo.2011.03.008. Epub 2011 Mar 15. PMID: 21444148; PMCID: PMC3085565.
Maserejian NN, Wager CG, Giovannucci EL, Curto TM, McVary KT, McKinlay JB. Intake of caffeinated, carbonated, or citrus beverage types and development of lower urinary tract symptoms in men and women. Am J Epidemiol. 2013 Jun 15;177(12):1399-410. doi: 10.1093/aje/kws411. Epub 2013 May 30. PMID: 23722012; PMCID: PMC3676152.
Nandy S, Ranganathan S. Urge incontinence. 2020 Sep 23. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 33085319.
Nijman RJ. Classification and treatment of functional incontinence in children. BJU Int. 2000 May;85 Suppl 3:37-42; discussion 45-6. doi: 10.1111/j.1464-410x.2000.tb16944.x. PMID: 11954196.
Nitti VW. The prevalence of urinary incontinence. Rev Urol. 2001;3 Suppl 1(Suppl 1):S2-6. PMID: 16985992; PMCID: PMC1476070.
Redshaw JD, Lenherr SM, Elliott SP, Stoffel JT, Rosenbluth JP, Presson AP, Myers JB; Neurogenic Bladder Research Group (NBRG.org). Protocol for a randomized clinical trial investigating early sacral nerve stimulation as an adjunct to standard neurogenic bladder management following acute spinal cord injury. BMC Urol. 2018 Aug 29;18(1):72. doi: 10.1186/s12894-018-0383-y. PMID: 30157824; PMCID: PMC6116487.
Saint S, Kaufman SR, Rogers MA, Baker PD, Ossenkop K, Lipsky BA. Condom versus indwelling urinary catheters: a randomized trial. J Am Geriatr Soc. 2006 Jul;54(7):1055-61. doi: 10.1111/j.1532-5415.2006.00785.x. PMID: 16866675.
Shaw JM, Nygaard IE. Role of chronic exercise on pelvic floor support and function. Curr Opin Urol. 2017 May;27(3):257-261. doi: 10.1097/MOU.0000000000000390. PMID: 28212118; PMCID: PMC5433620.
Singha P, Locklin J, Handa H. A review of the recent advances in antimicrobial coatings for urinary catheters. Acta Biomater. 2017 Mar 1;50:20-40. doi: 10.1016/j.actbio.2016.11.070. Epub 2016 Dec 1. PMID: 27916738; PMCID: PMC5316300.
Stampas A, Gustafson K, Korupolu R, Smith C, Zhu L, Li S. Bladder neuromodulation in acute spinal cord injury via transcutaneous tibial nerve stimulation: cystometrogram and autonomic nervous system evidence from a randomized control pilot trial. Front Neurosci. 2019 Feb 19;13:119. doi: 10.3389/fnins.2019.00119. PMID: 30837835; PMCID: PMC6390711.
Thomas LH, Coupe J, Cross LD, Tan AL, Watkins CL. Interventions for treating urinary incontinence after stroke in adults. Cochrane Database Syst Rev. 2019 Feb 1;2(2):CD004462. doi: 10.1002/14651858.CD004462.pub4. PMID: 30706461; PMCID: PMC6355973.