Upper Extremity Care
The shoulder, upper arm, forearm, and hand constitute the Upper Extremity. These body parts work in unison for function. With paralysis, the upper extremity is often used to accommodate function for other parts of the body. This can add additional stress and overuse to this body part that is not made for these additional challenges. Caring for your upper extremities is critical to maintaining your health and independence.
The components of the upper arm should work together for the best function. The main purpose of the use of the upper extremity is to allow free-flowing hand function. In other words, the arms support the positioning of the hands, the elbow brings the hand close to and away from the body, and the shoulder allows range of motion for the arm. The upper extremities serve to allow your hands a wide range of motion in all directions. There is the capacity to lift, pull or push.
There are many challenges to your upper extremities with paralysis. These include repetitive use or overuse arm issues and heavy lifting. Even though the structure of the arms is similar to the leg structure, the smaller arm anatomy is not made to carry the entire weight of the body. The much larger leg structure is used when walking or moving the body. Advancing age can be related to upper extremity issues as can a significant weight gain over time or even a temporary weight gain such as with pregnancy. Medical problems can increase arm dysfunction such as cardiac issues.
Prevention should be the first line of defense against upper extremity complications due to paralysis. Risk-reducing strategies can assist with avoiding or at least deferring the onset of upper extremity issues.
Anatomical components of the upper extremity include bones for structure, muscles for power, nerves for sensation and movement, blood vessels to provide oxygen and nutrients, and skin for protection and body temperature regulation.
Bones of the upper extremity consist primarily of skeletal structures including the shoulder (scapula), upper arm (humerus), forearm (radius and ulna), and hand bones, among others. There are joints that allow movement of the rigid bones. Tendons attach to the bones from the muscles.
Some issues that can occur to the bones after paralysis may include:
- Changes in posture including scoliosis and chest irregularities
- Decreased bone density (osteopenia/osteoporosis)
- Fractures (broken bones)
- Heterotopic Ossification (H.O.) (bone growth into the muscle)
- Olecranon bursitis (inflammation of the bursa over the olecranon of the elbow)
- Osteoarthritis (arthritis of the bones)
- Osteophytes (bone spurs)
- Pulling on joints
- Rotator cuff injury (a group of muscles in the shoulder)
- Shoulder dislocation
- Shoulder pain/injury
- Subluxation of the shoulder due to the dependent weight of the arm, poor positioning of the joint
- Shoulder impingement (rubbing of tendons in the shoulder)
Muscles in the upper extremity are skeletal muscles that attach to the bones to create movement. The main muscles in the upper extremity are noted in the diagram below. There are also skeletal muscles in the hand for fine motor function.
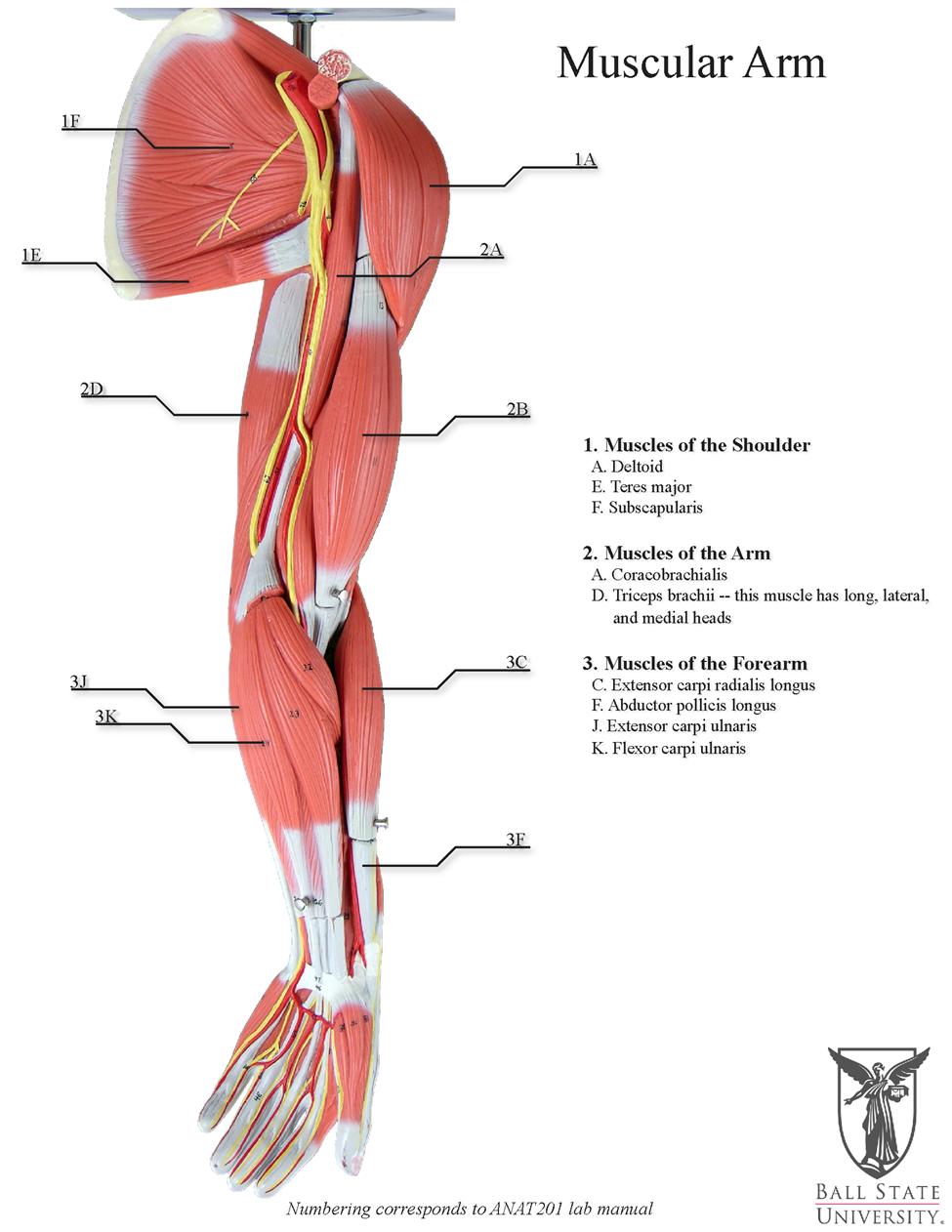
Graphic appears courtesy of Ball State University.
Issues of the upper extremity muscles after paralysis may include:
- Contractures (rigidity in muscles reducing movement in joints)
- Irritation of tissue connecting the muscle to the bone
- Lateral epicondylitis (tennis elbow)
- Muscle atrophy (shrinking)
- Muscle pain from the cervical and thoracic paraspinal muscles tendonitis
- Pain above the area of paralysis
- Rotator cuff injury (tendon injury in the shoulder)
- Scar tissue from repeated injury
- Tendonitis (inflammation of the tendons)
- Tone (Spasms)
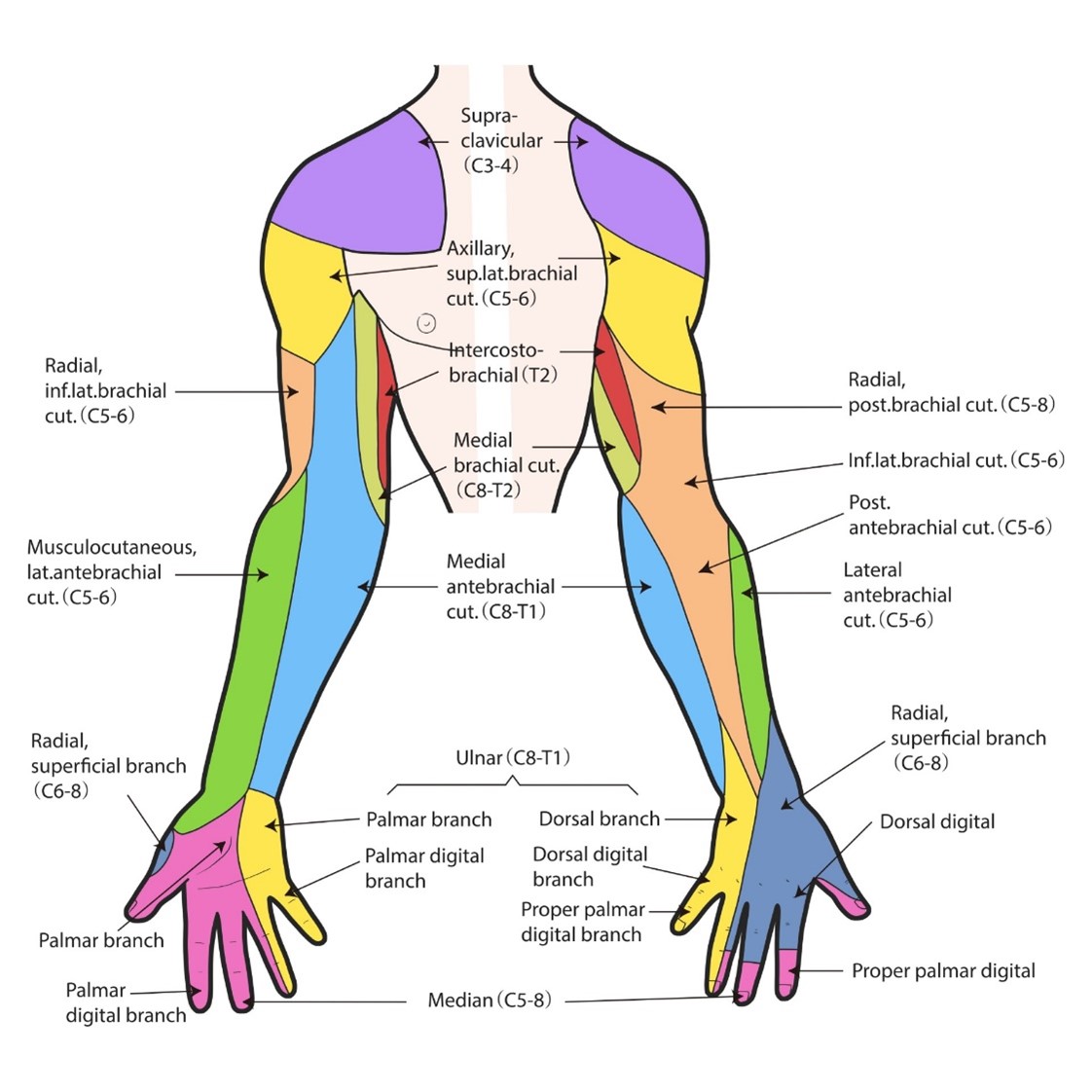
Nerves carry messages to and from the brain and body. Messages sent to the brain to the body for movement are motor nerves. Messages sent from the body to the brain are sensory nerves. This graphic shows the nerves that affect the parts of the upper extremity.
Issues with nerves after paralysis in the upper extremities may include:
- Movement–the ability to move the limb either partially or fully
- Nerve entrapment such as carpal tunnel syndrome (the most prominent in SCI) followed by ulnar nerve syndrome (also known as cubital tunnel injury), and brachial plexus injury in the shoulder area
- Sensation–the ability to feel or perceive feelings such as pain, itch, heat, cold, touching, and regulating body temperature among others
Blood Vessels are a part of the cardiovascular system that bring nutrients and oxygen to the cells of the body through the arteries. The veins remove cell waste through the veins. Small vessels that connect the arteries and veins are called arterials.
Issues that affect blood vessels after paralysis may include:
- Atherosclerosis–a build-up of plaque in the artery that narrows the path for blood flow
- Arm Artery Disease (a narrowing or blockage of the artery), a form of peripheral artery disease (PAD)
- Complications from dialysis
- Deep vein thrombosis from constrictions or clots anywhere in the blood vessels. One such risk is when ‘hooking’ your arm around your wheelchair
- Edema–swelling in the hand or arm, after paralysis most often from limb dependency and lack of movement
- Pressure Injury–loss of movement can create pressure from the bones within the body affecting blood flow and thereby reducing skin continuity
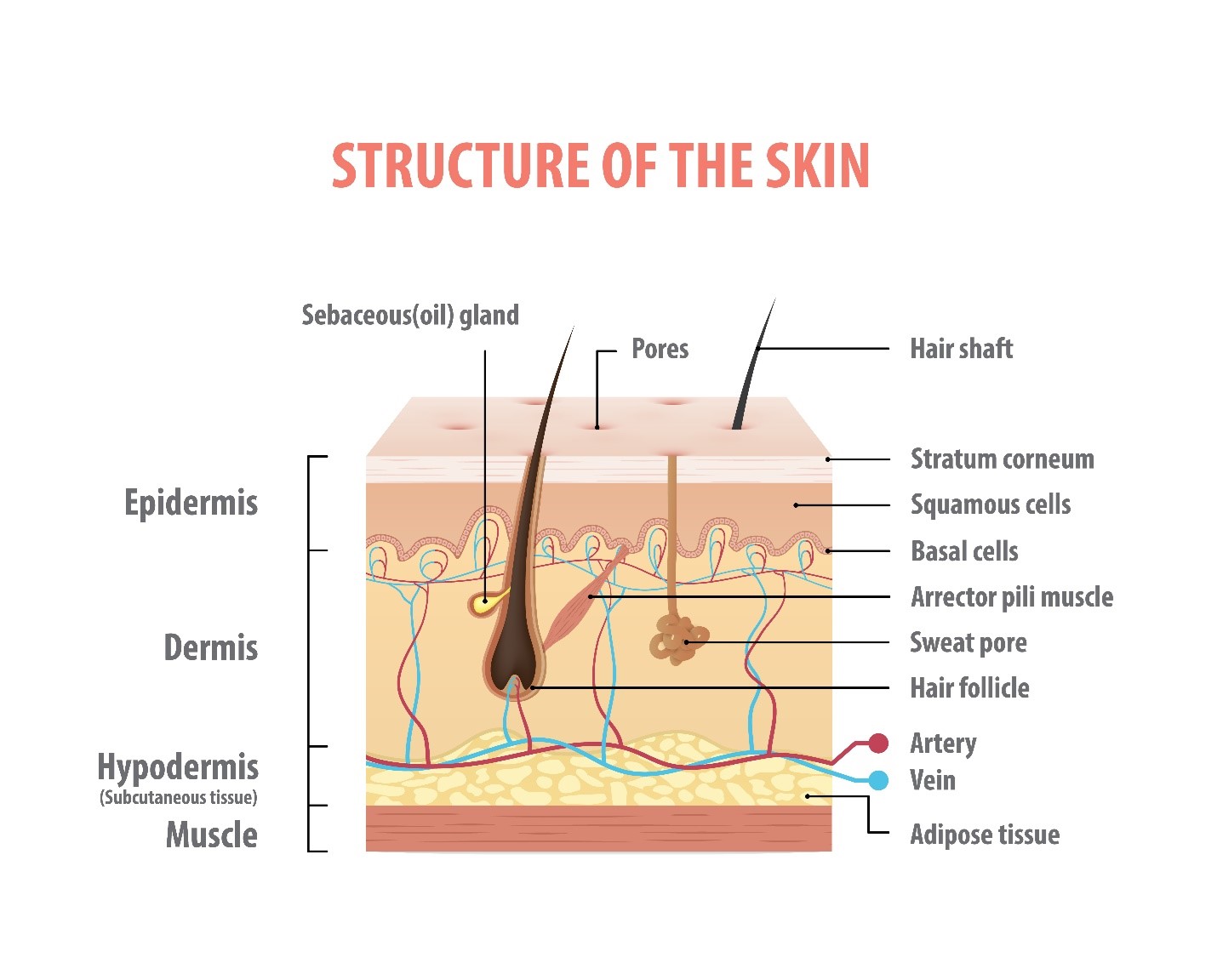
Skin of the upper extremity performs the same job as the skin on the rest of the body, which is to protect from dehydration, microorganisms, and ultraviolet light, as well as help to adjust internal body temperature regulation. The anatomical construction of skin is as in this graphic.
With paralysis, skin issues include:
- Callouses
- Dryness
- Irritation
- Pressure Injury
Symptoms/Diagnosis
Individuals with paralysis may first notice something physically different about the appearance in their upper arm. This may include a distortion in their usual anatomy including a misalignment, color change, swelling or open area of the skin, a change of absence of sensation where sensation is present, or a change in abilities. Muscle pain is usually felt by a sensation of stabbing, cramping, soreness, stiffness, and tone (spasms). Nerve pain may include sensations of stabbing, pins and needles, burning, or shooting sensations.
If sensation is affected, pain may be felt in an area with sensation adjacent to an insensate area or referred pain to another location such as the shoulder or jaw. Some individuals are not fully able to describe their pain due to sensation issues and may just report ‘something is wrong’.
Diagnosis begins with a complete physical examination including an ASIA examination of motor and sensory function to detect changes. Questions about pain include the effect on your sleep and mood.
How you have tried to modify your condition will be asked. This will include prescription medications, over-the-counter medications, recreational medications, movement, and prescribed and alternative therapies.
A review of equipment used for mobility and transfer will assess the appropriateness of assistive devices for your condition at the present time as opposed to the needs when it was prescribed.
An assessment of your technique of wheelchair propulsion will be made.
An evaluation through conversation of how daily activities are performed throughout the day and night will be discussed.
If you can sense pain, an assessment will be made of your description of the pain in your own words as well as using a pain assessment tool. Typically, pain is rated on a scale of 0-10 (0 representing no pain, 1 being the least pain, and 10 being the worst pain ever). The FACES scale is often used in pediatrics and for non-English speaking adults.
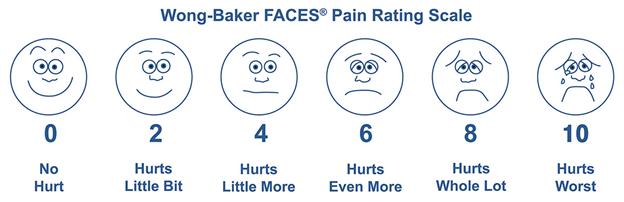
Graphic appears courtesy of Wong-Baker FACES Foundation.
Common testing includes X-ray for bone issues, CT or MRI for bone, muscle, and nerve concerns, and Electromyography/Nerve Conduction Studies (EMG/NCS) for muscle and nerve issues.
Treatments
How an issue with the upper extremity is treated depends on the source of the issue. Common treatments for the bones, muscles, nerves, blood vessels, and skin are listed below. It is important to note that issues in the upper extremity rarely appear in just one body system but will appear in several combinations so treatment is individualized to the specific needs of each person.
Bones Medical issues in the bones are treated mostly by therapy especially if diagnosed early. This may include:
- Adaptive equipment to reduce stress on joints, strengthening muscles, and exercises to keep joints supple.
- Gently performing stretching exercises helps keep the bones functioning.
- Proper positioning and use of positioning equipment are imperative to keep the skeleton in alignment.
- Ergonomic evaluations to assess movement and repetitive movements can assist with the prevention of bone injury.
- Electrical stimulation may be used to enhance muscle function, to help with bone healing, and to control pain.
- The use of a standing frame may improve bone density.
- Braces and splints may be needed to keep bones in alignment or to present further bone issues such as slowly releasing contractures, or for treatment of scoliosis.
- Some bone issues are treated with medications such as for improving bone density, for treatment of arthritis, and for reduction of heterotopic ossification.
- Injuries to the bones that cannot be treated with therapy may require surgery for correction. This occurs with fractured (broken) bones, scoliosis, and heterotopic ossification, among other concerns.
Heterotopic ossification (HO) occurs when bone cells grow outside of the bony skeleton into the muscle tissue, usually but not always at a joint. This leads to pain and difficulty in moving the affected joint. You may notice difficulty moving a joint, pain, referred pain, increased tone (spasms), or episodes of autonomic dysreflexia (AD). In advanced cases, you may see swelling in the area. Treatment in the early stages includes gentle mobilization of the joint. Anti-inflammatory medication (such as Indomethacin) may be provided for pain. HO is treated with medication such as Etidronate (Didronel) and others. Other treatments may include radiation therapy or targeted injections to the area. Advance cases require surgical removal to release the joint for movement. Removing HO may require reduction of muscle tissue so early treatment is recommended.
Shoulder subluxation becomes an issue with weak upper extremity muscles resulting in the weight of one or both unsupported arms pulling the ball out of the socket joint in the shoulder. This can occur in stroke, spinal cord injury, or other neurological diseases.
As in the graphic below, a physical assessment is made by placing a finger over the skin at the area of the shoulder at the junction of the acromion and articular surface of the humerus. There should be no separation of the joint in this area. If separation is present, it is measured by one finger, two fingers, or three or four-finger widths. This physical assessment would indicate X-rays are needed for further diagnosis. If sensation is present, pain may be felt, or if sensation is challenged, radiated pain to the jaw may be felt. Increased tone (spasms), or autonomic dysreflexia (AD) may appear or increase.
Early treatment or prevention is managed with proper positioning or with the use of a shoulder support brace. More advanced treatment includes the use of electrical stimulation to strengthen the muscles that support the shoulder. Later treatment can include surgical correction but this condition can be corrected if diagnosed early.
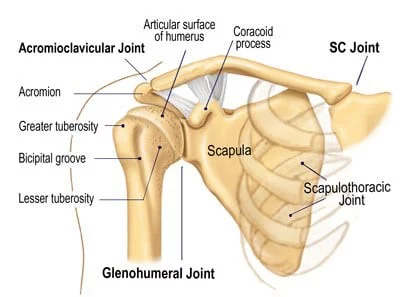
Graphic appears courtesy of Dalton Myoskeletal.
Muscles Pain in muscles in the upper extremity can be treated by resting the limb, elevation, or taking nonsteroidal anti-inflammatory medication if prescribed by your healthcare professional. These treatments are especially helpful to those individuals with a newer onset of paralysis as the muscles above the area of paralysis are now doing extra work to accommodate for less functional muscles. Therapy to strengthen the muscles improves this issue over time.
A cold, flu, stress, or even being overtired can lead to muscle aches and pains. Some neurological diseases can lead to muscle aches including multiple sclerosis, amyotrophic lateral sclerosis (ALS), muscular dystrophy, myasthenia gravis, spinal muscular atrophy, and fibromyalgia, among others. Scheduled rest and gentle movements can help reduce muscle pain symptoms. Gentle exercise may be best accomplished in a heated pool to avoid overexertion.
As functional use and overuse of the upper extremity can lead to pain, ergonomics of your mobility should be assessed. This includes movements such as transfers, wheelchair propulsion, and overreaching. Adaptions to your equipment may be needed. A manual wheelchair should be propelled beginning with your arm straight down at the side of your body, aligned with the axle as opposed to reaching back. Transfer assistive devices, wheelchair power assist propulsion equipment, and reorganizing frequently used items in your home for less overreaching are helpful to prevent these issues.
Rotator cuff injury can occur due to the overuse and extensive use of the shoulder for movement of the body. Symptoms may include pain or radiated pain to the jaw in the shoulder, and weakness or a change in strength in the arm. Treatment consists of resting the shoulder which can be challenging when depending on your shoulder to move your body. Therapy can assist with strengthening exercises of the muscles of the shoulder or electrical stimulation to strengthen the shoulder muscles. Steroid injections may be given to reduce swelling and pain. In more severe cases, rotator cuff surgery (usually arthroscopic) is needed which will require time for healing without use of the shoulder. In extreme cases, shoulder replacement or tendon transfers may be needed.
Bone and Nerve Tone (spasticity) can lead to pain for individuals with spasticity. Each of our muscles comes in a set that balances each other. One muscle in the set is for pushing and one is for pulling. The pulling muscles are slightly stronger which with paralysis can lead to contractures. Miscommunication of messages to muscles can create tone. Treatment for underlying issues should be considered to reduce pain such as for contractures, or tone (spasms) with gentle movement and stretching, medication, or Botox injections. Additional information about treatment of spasticity can be found here.
Neuromuscular stimulation both on the skin and surgically implanted has greatly increased the possibility of regaining function in the upper extremity. Many advances are occurring with more treatments readily available for everyone. In this treatment, an impulse is sent from a device through the nerves and muscles of the body to the brain to create movement and sensation.
Constraint Induced Movement Therapy and Mirror Therapy are being used as a treatment for stroke recovery. In this therapy, the non-affected arm is constrained forcing the affected limb to be used. This therapy is being studied with other neurological conditions to assess effectiveness. Mirror therapy involves looking at your limb in a mirror to improve movement from the non-involved side of the brain.
Tendon and Nerve Transfers can be surgically performed to increase the function of the arm and hand. Tendons can be relocated to increase strength. Nerves can be transferred, split, or grafted from one area with function to another area with less function. Nerves in the arms are peripheral nerves that can be relocated. These treatments require a specialist in hand surgery, neurosurgery, or reconstructive surgery. Recovery time and extensive therapy are required to re-educate the body to the new function.
A complete list of tendon transfers can be downloaded as a PDF here.
The article cited below has a chart that demonstrates upper extremity nerves that can be transferred and function that can be gained by level of injury.
Hawasli AH, Chang J, Reynolds MR, Ray WZ. Transfer of the Brachialis to the anterior interosseous nerve as a treatment strategy for cervical spinal cord injury: Technical note. Global Spine Journal 5(2):110-7, April 2015, DOI:10.1055/s-0034-1396760
Nerves Due to overuse of the upper extremity especially for mobility, nerve entrapments can occur. The locations for nerve entrapment in the upper extremity are in the brachial plexus, at the elbow (cubital tunnel syndrome), and at the wrist (carpal tunnel syndrome). Symptoms include nerve pain such as shooting pains, hypersensitivity, burning, tingling, and numbness. Early intervention includes a brace or splint worn at night. Adaptions for mobility using assistive transfer devices and assistive wheelchair propulsion can be used. Resting, not overstraining the nerve is critical to improvement in the early stages which can be a challenge to an individual with mobility issues. Later treatments include surgical intervention to release the entrapped nerve which will require no use for a period of time. This can greatly hamper mobility.
Neuropathic pain is pain specifically from nerve miscommunications. This pain can be quite severe. The pain experience is different for everyone. Early and ongoing treatment includes gentle movement to the extremity. Medication treatments include low-dose anti-epileptic and anti-seizure medicines, or medications specifically designed to treat neuropathic pain such as gabapentin (Neurontin) and pregabalin (Lyrica). The doses of these medications may be adjusted to effectively treat your pain or the dosage increased as your body becomes used to them. Advanced treatments include surgically implanted pain pumps, and nerve stimulators to break the pain message.
Blood Vessels Care of blood vessels is needed in the upper extremity to prevent deep vein thrombosis (blood clots) in the arms. Any constriction of the upper extremity such as splints, ace wraps, compression stockings on the arms, or bandages can lead to blood flow constriction within the arm causing a blood clot. It is necessary to have a blood clot assessed and treated immediately. Blood clots can break from their location in the arm and travel to the brain creating a stroke or to the lungs as a pulmonary embolism. Treatment includes anticoagulation medication. The Reeve Foundation’s DVT wallet card is available for you to alert healthcare professionals, caregivers, family members, and friends if you need emergency treatment for DVT.
Video: Deep Vein Thrombosis (DVT)
Edema is too much fluid in your body, especially the extremities, that should be returned to the heart and then removed from the tissues of the body. In paralysis, the blood vessels are not removing this fluid because of lack of movement and dependency of the limb. Elevation and an arm compression garment and compression glove are basic treatments. Fluid-reducing medications or a pump may be used in advanced cases to help push the fluid out of the arm tissues.
Skin After paralysis, the skin requires extra attention to maintain its ability to protect the body. Eating a healthy diet and drinking water within the restrictions of your bladder program is essential to feeding and hydrating skin.
Dry skin can lead to minute cracks and openings that can let in bacteria leading to infections. Dry skin on the hands, elbows, and any location that rubs can lead to a build-up of dead skin or callous. Do not pull off strips of dry skin, but wash with warm water, and apply an emollient lotion. Removing strips of dry skin leaves openings in the skin’s surface which can lead to infections.
A callous does not have the elasticity of healthy skin which can lead to breakdown, openings in the skin, and pain. Gently reduce callouses over time by soaking them daily with warm water and buffing the area with a wet washcloth. Apply an emollient lotion to the area. This process may take weeks to reduce the callous. Reducing the callous with an implement or too quickly can cut or overexpose the tender skin beneath the surface of the callous.
Pressure injury can occur anywhere on the arm including bony prominences, or where equipment rubs or constricts. A pigment change on the surface of the skin indicates a pressure injury has started. In darkly pigmented individuals, this pigment change may appear purplish or ashy. In lightly pigmented individuals, the pigment change is pinkish. Once the pigment change is seen on the surface of the skin, the unseen injury area under the skin is much larger and deeper. Treatment is to remove the pressure of equipment and to keep any pressure off the area by not leaning or putting body weight on it. If the skin is open, a dressing should be applied. An assessment by a healthcare professional is necessary for the specific treatment that is needed. More information about pressure injury prevention can be found in this blog.
Prevention of Upper Extremity Injury
Maintenance is essential to decreasing complications in the upper extremity.
- Positioning when in bed or when up assists with keeping the upper extremity in alignment, reduces the weight of pull through the joints, and can enhance function.
- Notice where your arm and hand are positioned to avoid trapping in your chair or other injuries.
- Keeping the hand and arm higher than your heart reduces edema as does compression arm and glove garments, and pump therapy.
- Ergonomic equipment assists with exercise, positioning, and function. Observe your living and workspace so you do not have to overreach or strain to get items.
- Transfer equipment can assist with the reduction of weight put through your arms. Even if just used at home, the number of transfers using your arms is greatly reduced.
- Wheelchair propulsion should be done with the arm straight down along the side of the body, above the wheel axle, then moved forward.
- Perform routine exercise to keep your arm in good condition either by moving it yourself or having someone move it for you.
- Look at your arms to assess for pigment changes of pressure injury, openings in the skin, and swelling that can indicate a deep vein thrombosis, edema, broken bone, or other injury.
- Listen for crackles and feel for movement that is not smooth to assess for bone injury or development of arthritis, contractures, heterotopic ossification, or shoulder subluxation.
- Report any pain symptoms that could indicate nerve entrapment, sore muscles, or tone (spasms).
Video: Preventing Shoulder Issues
Is your wheelchair set up for maximum efficiency? You could be working too hard to get around and setting yourself up for shoulder pain.
History
Upper extremity care has evolved slowly over time. In the days when rehabilitation began with a huge leap in developing after World War II, the upper extremity was thought of as a replacement for mobility if the legs were injured. Early publications about the upper extremity VVafter paralysis appeared sporadically with the first push of knowledge in the late 1970s. It was in the early 2000s that acknowledgment of issues and treatments was more prevalent in research, although well-known in the community.
In the 1990s increased research of overuse injury has led to developments in wheelchair propulsion and transfer techniques for reducing the stress of the upper extremity. These techniques and equipment have assisted individuals with paralysis to reduce injury and have longer functional use of their limbs.
In the early 2000s, the development of an implantable functional electrical device made independent upper extremity function after paralysis a possibility. These early devices included extensive surgery and were a bit difficult for the user to coordinate and maintain although function was improved. With the advent of transdermal functional electrical stimulation, the use for functional movement in the upper extremity has greatly increased. Devices are being released by several companies that are revolutionizing upper extremity function.
New research of internal stimulation of the vagus nerve is producing improved upper extremity function.
Currently, healthcare professionals recognize the importance of maintaining upper extremity health. More individuals are able to obtain transfer equipment to help preserve function especially while aging.
Facts and Figures
In a study by M. Dalyan, DD Cardenas, and B Gerard (1999) titled Upper Extremity Pain after Spinal Cord Injury, 58.5% of individuals reported upper extremity pain.
Carpal tunnel syndrome is the most reported nerve entrapment injury reported with spinal cord injury.
Resources
If you are looking for more information about upper extremity care or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 7:00 am to 12:00 am midnight EST.
Check out our repository of on hundreds of topics ranging from state resources to secondary complications of paralysis. We encourage you to reach out to support groups and organizations, including:
The Christopher & Dana Reeve Foundation’s Peer & Family Support Program can match individuals with paralysis with a peer mentor. It also offers caregiver to caregiver mentoring.
Clinical Guidelines
Stroke Foundation, Upper Limb Management After Stroke.
References
Akkurt H, Karapolat HU, Kirazli Y, Kose T. The Effects of Upper Extremity Aerobic Exercise in Patients with Spinal Cord Injury: A Randomized Controlled Study. Eur J Phys Rehabil Med. 2017 Apr;53(2):219-227. doi: 10.23736/S1973-9087.16.03804-1. Epub 2016 Nov 8. PMID: 27824234.
Chow JW, Levy CE. Wheelchair Propulsion Biomechanics and Wheelers’ Quality of Life: An Exploratory Review. Disabil Rehabil Assist Technol. 2011;6(5):365-77. doi: 10.3109/17483107.2010.525290. Epub 2010 Oct 11. PMID: 20932232.
Dalyan M, Cardenas DD, Gerard B. Upper Extremity Pain after Spinal Cord Injury. Spinal Cord. 1999 Mar;37(3):191-5. doi: 10.1038/sj.sc.3100802. PMID: 10213328.
De Miguel-Rubio A, Rubio MD, Alba-Rueda A, Salazar A, Moral-Munoz JA, Lucena-Anton D. Virtual Reality Systems for Upper Limb Motor Function Recovery in Patients with Spinal Cord Injury: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth. 2020 Dec 3;8(12):e22537. doi: 10.2196/22537. PMID: 33270040; PMCID: PMC7746495.
Dost G, Dulgeroglu D, Yildirim A, Ozgirgin N. The Effects of Upper Extremity Progressive Resistance and Endurance Exercises in Patients with Spinal Cord Injury. J Back Musculoskelet Rehabil. 2014;27(4):419-26. doi: 10.3233/BMR-140462. PMID: 24614829.
Etoom M, Hawamdeh M, Hawamdeh Z, Alwardat M, Giordani L, Bacciu S, Scarpini C, Foti C. Constraint-Induced Movement Therapy as a Rehabilitation Intervention for Upper Extremity in Stroke Patients: Systematic Review and Meta-Analysis. Int J Rehabil Res. 2016 Sep;39(3):197-210. doi: 10.1097/MRR.0000000000000169. PMID: 27123790.
Gohritz A, Fridén J. Management of Spinal Cord Injury-Induced Upper Extremity Spasticity. Hand Clin. 2018 Nov;34(4):555-565. doi: 10.1016/j.hcl.2018.07.001. Epub 2018 Aug 20. PMID: 30286970.
Grampurohit N, Bell A, Duff SV, Mulcahey MJ, Thielen CC, Kaplan G, Marino RJ. Highlighting Gaps in Spinal Cord Injury Research in Activity-Based Interventions for the Upper Extremity: A Scoping Review. NeuroRehabilitation. 2021;49(1):23-38. doi: 10.3233/NRE-210042. PMID: 33967071.
Hawasli AH, Chang J, Reynolds MR, Ray WZ. Transfer of the Brachialis to the Anterior Interosseous Nerve as a Treatment Strategy for Cervical Spinal Cord Injury: Technical Note. Global Spine Journal 5(2):110-7, April 2015, DOI:10.1055/s-0034-1396760
Huang J, Ji JR, Liang C, Zhang YZ, Sun HC, Yan YH, Xing XB. Effects of Physical Therapy-Based Rehabilitation on Recovery of Upper Limb Motor Function after Stroke in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ann Palliat Med. 2022 Feb;11(2):521-531. doi: 10.21037/apm-21-3710. PMID: 35249330.
Ikbali Afsar S, Mirzayev I, Umit Yemisci O, Cosar Saracgil SN. Virtual Reality in Upper Extremity Rehabilitation of Stroke Patients: A Randomized Controlled Trial. J Stroke Cerebrovasc Dis. 2018 Dec;27(12):3473-3478. doi: 10.1016/j.jstrokecerebrovasdis.2018.08.007. Epub 2018 Sep 5. PMID: 30193810.
Inanici F, Brighton LN, Samejima S, Hofstetter CP, Moritz CT. Transcutaneous Spinal Cord Stimulation Restores Hand and Arm Function After Spinal Cord Injury. IEEE Trans Neural Syst Rehabil Eng. 2021;29:310-319. doi: 10.1109/TNSRE.2021.3049133. Epub 2021 Mar 2. PMID: 33400652.
Israely S, Leisman G, Carmeli E. Improvement in Arm and Hand Function after a Stroke with Task-Oriented Training. BMJ Case Rep. 2017 Mar 17;2017:bcr2017219250. doi: 10.1136/bcr-2017-219250. PMID: 28314812; PMCID: PMC5372193.
Jung KM, Choi JD. The Effects of Active Shoulder Exercise with a Sling Suspension System on Shoulder Subluxation, Proprioception, and Upper Extremity Function in Patients with Acute Stroke. Med Sci Monit. 2019 Jun 30;25:4849-4855. doi: 10.12659/MSM.915277. PMID: 31256191; PMCID: PMC6618341.
Lu X, Battistuzzo CR, Zoghi M, Galea MP. Effects of Training on Upper Limb Function after Cervical Spinal Cord Injury: A Systematic Review. Clin Rehabil. 2015 Jan;29(1):3-13. doi: 10.1177/0269215514536411. Epub 2014 Jun 4. PMID: 25575932.
Qi L, Zhang L, Lin XB, Ferguson-Pell M. Wheelchair Propulsion Fatigue Thresholds in Electromyographic and Ventilatory Testing. Spinal Cord. 2020 Oct;58(10):1104-1111. doi: 10.1038/s41393-020-0470-2. Epub 2020 May 4. PMID: 32367012.
Smith BW, Bueno DR, Zondervan DK, Montano L, Reinkensmeyer DJ. Bimanual Wheelchair Propulsion by People with Severe Hemiparesis after Stroke. Disabil Rehabil Assist Technol. 2021 Jan;16(1):49-62. doi: 10.1080/17483107.2019.1630018. Epub 2019 Jun 28. PMID: 31248296.
Symonds A, Barbareschi G, Taylor S, Holloway C. A Systematic Review: The Influence of Real Time Feedback on Wheelchair Propulsion Biomechanics. Disabil Rehabil Assist Technol. 2018 Jan;13(1):47-53. doi: 10.1080/17483107.2016.1278472. Epub 2017 Jan 19. PMID: 28102100.
Vanlandewijck Y, Theisen D, Daly D. Wheelchair Propulsion Biomechanics: Implications for Wheelchair Sports. Sports Med. 2001;31(5):339-67. doi: 10.2165/00007256-200131050-00005. PMID: 11347685.
Ward JA, Power DM. Nerve Transfers Following Cervical Spinal Cord Injury: A Review and Reconstructive Algorithm. Journal of Musculoskeletal Surgery and Research, 2019: 3:1;152-160.
Zhuang JY, Ding L, Shu BB, Chen D, Jia J. Associated Mirror Therapy Enhances Motor Recovery of the Upper Extremity and Daily Function after Stroke: A Randomized Control Study. Neural Plast. 2021 Sep 29;2021:7266263. doi: 10.1155/2021/7266263. PMID: 34630560; PMCID: PMC8494575.
F