Respiratory Health
Breathing is controlled by the autonomic nervous system (ANS), the part of the nervous system that acts automatically or outside of your conscious control. The interesting thing about breathing is that you can also voluntarily affect it by consciously taking a deep breath, coughing and holding your breath. Most ANS controlled body systems do not allow a conscious ‘override’ of function. Along with automatic control, having some conscious effect on breathing shows the importance of maintenance of this system.
Air is taken in by the lungs, or inhaled, for the purpose of extracting oxygen from the air. Oxygen passes through tiny vessels in the lungs called alveoli. The alveoli allow oxygen molecules to pass into the bloodstream. The oxygen molecule is then distributed to all cells in the body. When oxygen is metabolized by the body, carbon dioxide is released into the blood. The carbon dioxide waste is carried back to the lungs where it is exhaled back into the air.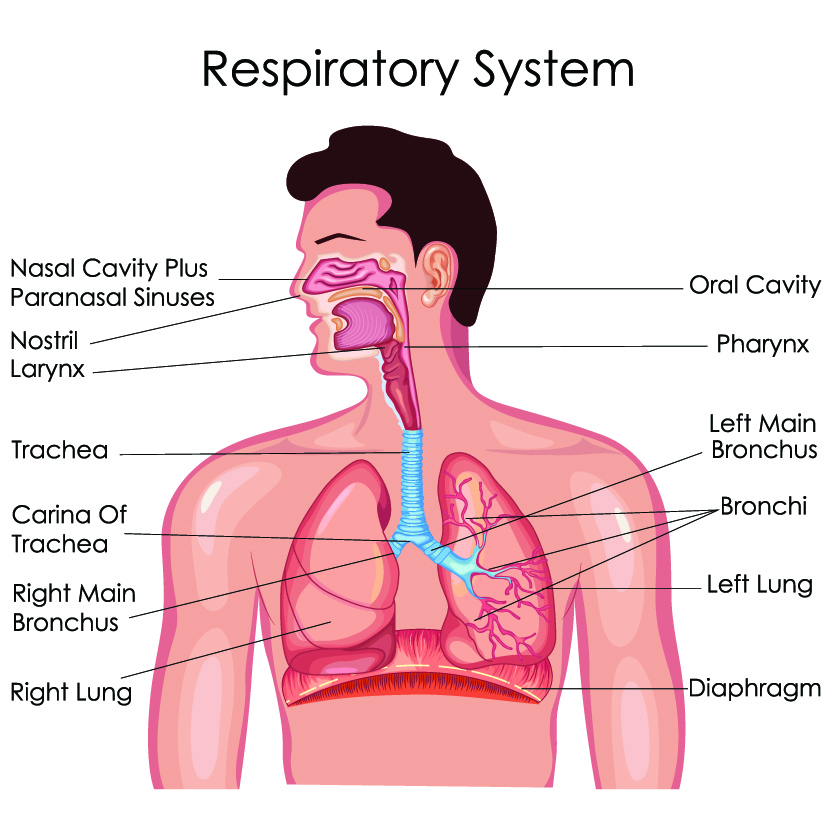
Breathing is controlled by several factors. The main central nervous system (CNS) control of breathing is in the brainstem. Spinal cord injury or a stroke in the brainstem often affects breathing. Major nerves involved in respiration include the phrenic nerve, vagus nerve, and posterior thoracic nerves.
The diaphragm is responsible for pulling the lungs down in the body to draw air in. The diaphragm is controlled by the phrenic nerve that exits the spinal cord at levels C3, C4 and C5. An injury at these levels will affect diaphragm control of breathing. A second set of muscles, the intercostal muscles, assist in causing air to enter the lungs. The intercostal muscles are in between each rib. These muscles cause the lungs to draw outwardly, around the lung. They do this by raising the ribs upward and outward assisting in bringing air into the lungs. The intercostal muscles are controlled by spinal nerves T1 to T11. A spinal cord injury that includes these levels will affect the functional ability of the intercostal muscles. A third set of muscles also assist with drawing air into the lungs by creating a negative pressure in the lungs are the abdominal muscles. These muscles are controlled by spinal nerves T7 to L1. A spinal cord injury that includes these levels will affect some intercostal muscles and abdominal muscles. Other muscles including those in the neck also assist with breathing.
To exhale air, the muscles that bring air into the body relax. This relaxation of the muscle groups causes the lungs to return to their restful size thereby pushing air out of the body. Deoxygenated air and carbon dioxide pass out of the body. Breathing in can only be accomplished by activation of the muscles but release of air from the lungs does not require the muscles to work, they just relax, and air is expelled. Muscles do not automatically push air out. You can consciously activate your muscles to force air out of the body, but air will flow out automatically in the natural breathing process.
Acute Respiratory Issues after Spinal Cord Injury
After spinal cord injury, several aspects of breathing can be affected. Depending on the level of injury, the autonomic nervous system (ANS) that controls automatic ability of breathing is affected. The conscious ability to control breathing is affected such as the ability to take a deep breath to open the air passages in the lungs and/or to cough, the respiratory system’s protective mechanism. The strength of muscle function to take in air is affected at the level of the injury and below. Tone (spasticity) can affect the relaxation of the three sets of breathing muscles complicating breathing in and out. Speech can be altered.
If paralysis occurs in C2 or higher, the phrenic nerve is affected and therefore the diaphragm does not function. Mechanical ventilation will be required to facilitate breathing. Due to advancements in SCI respiratory care, an individual with a spinal cord injury at C3 or C4 may be able to learn to breathe without the use or with partial use of mechanical ventilation. At these two levels, the diaphragm may retain some function but the intercostals, other chest wall muscles and abdominal muscles may not provide the integrated expansion of the upper chest wall as the diaphragm descends during inspiration.
During spinal shock in higher level injuries, the initial phase after spinal cord injury, the flaccid intercostal muscles cause the chest wall to sink in when the intercostal muscles should be pulling out. This imbalance can lead to less efficient breathing, airway collapse, more workload to breathe and small collapses of the sacs of the lungs. The breathing muscles can become stiff making recovery for respiration slower. Spasticity of the muscles can set in either reducing the effective ability to breathe or making breathing even stronger due to overactivity. During the acute phases of SCI, injury level may advance higher or lower depending on continuation or resolution of swelling or bleeding.
Individuals with paralysis at the mid-thoracic level and higher may have trouble taking a deep breath and exhaling forcefully. Because they may not have use of abdominal or intercostal muscles, these individuals also lose the ability to force a strong cough. This can lead to lung congestion and respiratory infections.
Chronic Respiratory Issues after Spinal Cord Injury
The three most common respiratory complications after spinal cord injury are:
- Atelectasis is a collapse of a lobe or the entire lung or even both lungs. This is due to either fluid building up in the tiny sacs (alveoli) where oxygen exchange occurs or the collapse of the sacs. In either condition, oxygen cannot be extracted from inhaled air because the sac is not functional. Symptoms include trouble breathing or shortness of breath, increased heart rate, coughing, a bluish color of your nail beds or lips. Chest pain is a hallmark symptom. This might not be felt if you have decreased sensation in your chest. You may have referred pain or episodes or new onset of autonomic dysreflexia (AD).
- Pneumonia is a condition where the sacs (alveoli) that exchange oxygen into the body, become filled with fluid or pus. It is an infection caused from bacteria, virus or fungi entering the respiratory system. Symptoms include a productive cough (a cough with phlegm), fever, chills and difficulty breathing.
- Respiratory Failure occurs when your body is not getting enough oxygen, is unable to eliminate carbon dioxide or a combination of both. It can be caused by a variety of reasons including pneumonia, opioid overdose, stroke, lung injury or disease or as a secondary consequence of spinal cord injury. Symptoms include difficulty breathing, feeling confused, a bluish color on your skin or lips. You might not notice these symptoms, but a caregiver should. Call 911 immediately.
Other respiratory issues that affect individuals with spinal cord injury are:
Cough is affected in relationship to the higher levels of spinal cord injury. Obtaining a strong cough can be difficult with more muscles involved that affect cough production. Coughing is a defense of the respiratory system that produces enough wind to pass through the lungs to remove debris that may have entered the respiratory system. It is a natural mechanism for cleaning the lungs.
Positioning affects lung function. Sitting is good for lung function as the diaphragm can be aided by gravity. However, sitting can also be a detriment if an abdominal binder is not used as the contents of the abdomen might not be contained due to lax abdominal muscles. This causes increased pressure in the abdominal cavity when sitting, which affects the ability of the diaphragm to work.
Pulmonary edema (fluid in the lungs) occurs in 50% of individuals with onset of tetraplegia due to fluid resuscitation. Later in the injury, pulmonary edema can develop with cardiac complications, fluid overload or edema from ongoing ineffective cardiac function. Failure to use an abdominal binder increases the risk of development.
Pulmonary thromboembolism (P.E.) (blood clot or air bubble in the lungs) also occurs from poor cardiac function leading to poor circulation, lack of movement and constrictions. The clot typically forms elsewhere in the body and travels to the lung.
Other Respiratory Diagnoses
Adult Respiratory Distress Syndrome (ARDS)-a chronic build up of fluid in the sacs of the lungs (alveoli)
Aspiration-inhalation of fluid or food into the respiratory tract with an inability to clear it
Bronchitis-inflammation of the bronchi or the main tubes in the lungs
Bronchospasm-spasm of the bronchi which tighten the airway making it difficult to inhale or exhale
Lung abscess-a large pocket of infection in the lung
Pleural effusion-when the lung rubs directly on the membrane that contains it, causing significant pain
Pneumo/hemothorax-blood and/or gas collected in the membrane that contain the lungs
Pulmonary edema– excess fluid in the lungs
Tracheitis-an infection of the trachea, the main breathing pathway in the body, from the mouth to the lungs
Upper Respiratory Infection (URI)-an infection in the airways but not in the lungs (Most commonly, a cold)
Ventilatory failure-any inability of the respiratory system to function which is bringing in oxygen and eliminating carbon dioxide from the body
Pre-existing or development of respiratory disorders can compound difficulty in breathing after SCI. Many individuals have pre-existing respiratory conditions or new onset of respiratory conditions. These illnesses create an additive effect for breathing difficulty after spinal cord injury. Treatment for respiratory diseases must continue or sometimes need advancement in care to maintain respiratory health. Some conditions that affect breathing include asthma, COPD, chronic bronchitis, emphysema, lung cancer, cystic fibrosis, pleural effusion (the lung rubs against the membrane that contains it causing pain).
Sleep Apnea
Sleep Apnea is a respiratory sleep disease where a person stops breathing or breaths ineffectively during sleep. This can be for short periods of time. It can consist of complete breathing absence or difficulty breathing as demonstrated by snoring. You might not know that you are having difficulty because you will not notice while you are sleeping. Generally, someone else tells you that you snore or that you have stopped breathing for periods of time during sleep or that you gasp for air. You might notice symptoms of waking with a headache, dry mouth, irritability, an inability to concentrate, tiredness during the day or even falling asleep during the day.
There are three types of sleep apnea. Obstructive sleep apnea is the most common. It occurs due to throat muscles relaxing which does not let air pass through. Central sleep apnea occurs when the message from the brain to breath does not get through to the body. A combination of both types of sleep apnea is called Complex Sleep Apnea Syndrome. Individuals with spinal cord injury might have any of the three types.
Sleep apnea is significantly more common in people with spinal cord injuries. It is common in those with tetraplegia, with an estimated 25-40 percent having the condition. Respiratory muscle weakness is very likely involved at any level of injury. Obesity, particularly in the neck and abdomen, is also a risk factor for sleep apnea. Sleeping on your back is the most susceptible position for sleep apnea. Certain muscle relaxation medications (baclofen, for example, is known to slow down breathing) affect sleep patterns.
A sleep study is the assessment for sleep apnea. In this setting, you are monitored while sleeping. With spinal cord injury, you will want to ensure that the bed surface accommodates your needs and that your physical care needs will be provided prior to the study.
Treatment includes devices to maintain breathing while sleeping. This includes night sleeping and napping if needed during the day. Continuous positive airway pressure (CPAP) is a device that delivers air pressure through a mask to keep airways open during sleep. It is the most commonly used treatment. Alternatives include bilevel positive airway pressure (BPAP), a device that delivers more pressure with inhalation and less pressure as you exhale. A newer device is Adaptive Servo-Ventilation (ASV). This airflow device mimics the pattern of your normal breathing to replicate your breathing pattern when sleeping. It is recommended only for some types of sleep apnea. Oral appliances to physically open the airway when sleeping have also been used for some individuals depending on type of sleep apnea. Oral appliances are the least effective but do work for some individuals.
Assessment of the Respiratory System
The first step in finding the right treatment for respiratory issues is to establish the nature of the situation. The specifics of health care needs after a spinal cord injury are different for everyone.
Physical assessment is the first assessment of the respiratory system. A visual measurement of number of breaths per minute is the starting point. Normal breathing is 12 to 20 breaths per minute. Breathing trouble is noted if breaths are less than 12 per minute or over 25 breaths per minute for sustained periods, not just temporarily due to exertion. An increased number of breaths taken per minute indicate that more oxygen is needed in the body.
A healthcare professional will listen to your lungs using a stethoscope. This provides information about the quality of air moving through all lobes of the lungs. Absence of breathing, decreases in breaths or extra noises such as crackles and wheezes are noted.
The amount of oxygen that is in your blood can be measured with a pulse oximeter (SpO2). This is a little clip that is placed on your finger typically while your vital signs are being assessed in a medical appointment or you may have had a finger pad type placed for long term assessment while in the acute care hospital. The amount of light from the device that is absorbed through your finger provides the reading. Normal is between 100% and 95%. A low reading is at or under 90%.
A health history and family history will be done to see if there are any breathing issues that you may have such as respiratory illnesses of asthma, COPD, sinus issues, chest injury, surgery or any health concerns that may have an impact on your breathing. You will also be asked about any inhalants that you use such as smoking, vaping or non-medically prescribed inhaled drug use that will affect your body’s oxygenation.
The tissues (skin) of your body should all be healthy and your natural color. Respiratory issues can be noted if there is a bluish tinge to your lips or nails. The darker the blue pigment indicates a more significant breathing issue or a longer time of breathing trouble. The bluish pigment is an indication that oxygenation is not taking place in your body. The first symptoms of color change happen in the parts of the body furthest from your heart, as in toes and fingers or in areas of high capillaries concentrations such as your lips.
Grunting with breathing, nasal flaring (nostrils opening wide with inspiration), wheezing, or retraction of the chest or abdomen are all physical signs that an individual is making extra effort to draw air into the lungs. In usual respirations, you will see the chest rise and fall but typically, there are no extra sounds or muscle movement required to bring air into the body.
Sweating without fever or feeling warm indicates a person’s body is working hard. This can be due to the extra effort of needing to work to inhale air. A person who leans forward to breathe is really struggling for air. This is a sign that they may be heading toward a respiratory collapse.
Laboratory testing is used to assess the internal function of the body. Common lab tests for breathing include a complete blood count (CBC) which measures many indicators including hemoglobin, a protein that transports oxygen around the body. You need to breathe in oxygen but once inside your body, hemoglobin will move the oxygen around to be used by the cells. It also helps carry some carbon dioxide out of the body.
Blood gases (PaO2) are most often drawn from an artery at the wrist. This test assesses oxygenation in the body at the time of the blood draw. This is very similar to the pulse oximeter assessment except it does involve obtaining blood from inside the body.
Lung assessments are physical tests to view the lungs or to check their effectiveness. A chest X-ray provides a picture of what your lungs look like. This is a useful tool to see if there is an infection in the lungs such as pneumonia or blockage in the lungs. It also can be used to assess the basic structure of the lungs as well as to see the size of the lungs. A CT scan or MRI provides even more detailed information.
Peak Flow Meters are handheld devices that measure the force of exhalation (breathing out).
A pulmonary function test is an assessment of your lung function. This includes a spirometry where you force as much air into your lungs and exhale as much as you can. The amounts are measured. Also, the examiner will assess how easy it is for you to do this.
Electromyography (EMG) can be used to assess muscles response to nerve stimulation for movement in your chest and abdomen. A nerve conduction study (NCS) assesses nerve function. Both are useful in determining the presence of spasticity in respiratory nerves and muscles. An EMG/NCS can assess the diaphragm’s function and other nerves that assist with breathing.
Treatment of the Respiratory System after Spinal Cord Injury
All individuals with spinal cord injury from illness or disease at any level should pay close attention to keeping their respiratory system in the best condition possible. Anyone with spinal cord injury can develop respiratory conditions. The following information will help you maintain your respiratory system.
Keep your mouth clean. This is the number one activity to maintain lung health for everyone with or without a spinal cord injury. Oral hygiene has been heavily researched. Food particles that remain in your mouth or between your teeth start to decay after even a short amount of time. Saliva is working on the particles to break them down as one of the first steps in digestion. If you accidentally inhale or choke on the decayed food particle, you have bacteria entering your respiratory system. If you keep your mouth clean, but happen to choke, there should be no food particles in your mouth and if there is, the food particle will have less bacteria if any at all. There is much less risk of a lung infection if clean food accidentally enters your lungs. Maintain your oral health by cleaning your mouth, rinsing, flossing and keeping scheduled dental appointments. If you cannot swallow or have choking precautions, a toothbrush attached to suction is available.
Drink fluids to maintain moisture in your body. Hydration of the body keeps all systems working effectively especially in the respiratory system by keeping your lungs moist, mucous thin and easier to cough up.
Eat a well-balanced diet. Watch your intake to maintain your weight. This might be adding calories to avoid being too thin or lowering your calories to reduce some pounds. Extra pounds can collect especially in the neck area can make breathing more difficult or lead to sleep apnea. Poor abdominal muscle function creates negative pressure in the abdomen which affects the ability of the diaphragm to work at top efficiency.
Position yourself properly and in alignment. Sitting to one side or nodding off with your head forward can obstruct your breathing. Have someone listen to your breathing when you sleep, especially on your back, to check for sleep apnea.
Exercise your body. This can be accomplished by your moving your body parts both with and without sensation or having someone provide exercise to your body. Involvement in activity stimulates the body and may cause you to take deeper breaths to clear your lungs.
Deep breathe and cough. Take in three breaths as deeply as you can, then cough. This gets any secretions moving in your lungs. Once secretions are loosened, they are easier to move out. If you are unable to cough, use one of the non-invasive respiratory assistive devices listed below. If you use mechanical ventilation, use the sign button if allowed by your healthcare provider.
Use an abdominal binder. This is an external device that supports the abdominal muscles making breathing and coughing more efficient.
Stop smoking, vaping, or any non-medical inhalants or being around others who do. These substances fill your lungs so oxygen cannot get into your body. Not only are you addicting yourself to these substances, but you are not getting the oxygen needed to maintain your health. The results are pressure injury, poor circulation, heart and lung disease. Smoking causes cancer of the lungs, esophagus, larynx, mouth, throat, kidney, bladder, liver, pancreas, stomach, cervix, colon, rectum, and acute myeloid leukemia. There is medical assistance to aid your efforts to stop smoking available through your healthcare provider.
Get vaccinated and keep up to date on them. Obtain your flu shot yearly. The pneumonia vaccine is given every 10 years. These are necessary to reduce your risk of contracting these dangerous diseases.
Breathing Assistance
At times, mechanical assistance can help your breathing after spinal cord injury. Just as with sleep apnea, there are many ways to aid breathing. The choice of breathing assistance devices should be made with input from your healthcare professional for best results.
Non-invasive Respiratory Assistance
Use a bulb syringe to keep the nose and back of the mouth clear of secretions. This is very helpful if you have difficulty blowing your nose.
For mild congestion, drink steamy liquids, breathe moist air such as being in a room with a steamy shower, or use a humidifier. Steam thins mucous.
An incentive spirometer is used to expand the airway and lungs. When you inhale, a series of small plastic spheres in the device will elevate. The goal is to increase the sphere’s elevation and to hold them steady which exercises your lungs providing a deep breath.
Other respiratory muscle training exercises might be taught by a respiratory or physical therapist.
Abdominal binders strengthen contractions of the abdominal muscles to improve respiratory function.
There are several techniques that can be used to loosen mucous and congestion in the lungs.
- Percussion or a light drumming on the rib cage can help loosen congestion.
- The Flutter is a handheld device used to loosen mucus from the lungs. It looks somewhat like an asthma inhaler. A steel ball inside the device causes vibration inside the airway and lung walls. This can be performed by individuals even with limited hand function.
- Postural drainage uses gravity to move secretions from the bottom of the lungs to higher in the chest where it can be coughed up. This usually works when the head is lower than the feet for 15-20 minutes. Be sure to check with your healthcare professional prior to attempting this maneuver.
- Glossopharyngeal breathing can be used to help obtain a deeper breath, by “gulping” a rapid series of mouthfuls of air and forcing the air into the lungs, and then exhaling the accumulated air. It can be used to help with coughing.
- Cough assist by a caregiver is used by some individuals. This can be harmful if not done properly. Check with your healthcare provider to ensure it is safe at your level of injury and that the person educated to perform the function is doing it properly. Improper cough assist can lead to a variety of serious health issues.
Medications
Mucolytics are medications that aid in the clearing of airways, lungs, bronchi and trachea, including:
Guaifenesin and other expectorants are pills or liquids that can be taken to thin mucous in the respiratory system. Some individuals take this occasionally when needed while others maintain a regular schedule.
Nebulized sodium bicarbonate is frequently used to make tenacious secretions easier to eliminate.
Nebulized acetylcysteine is also effective for loosening secretions, although it may trigger reflex bronchospasm.
Non-Invasive Ventilation (NIV) is typically used for acute respiratory dysfunction (ARD) or acute respiratory failure (ARF) but can also be used for long term breathing.
If an individual is not getting enough oxygen without a structural problem in the body, oxygen might be provided through a nasal tube. This can be by using low flow or high flow nasal cannula, the two-pronged tube that releases oxygen just barely into the nose. When using this technique, the mouth should be able to be closed most of the time to get the full effect of the oxygen. If unable to keep the mouth closed, a mask over the nose and mouth might be used or the upper body could be placed in a tent over the bed.
Continuous Positive Airway Pressure (CPAP) is an external breathing device (NIV) that fits over the nose and sometimes also the mouth. There are several versions of this treatment including nasal Continuous Positive Airway Pressure (nCPAP) and Bubble Continuous Positive Airway Pressure (BCPAP). Each have differences but in general they gently blow in condensed air to keep the nose, airway and lungs open. You have probably heard about this treatment for adults who have obstruction in their airway when sleeping (sleep apnea). These devices might be used for breathing while sleeping to give the body a rest or all day to keep the airway open and air or oxygen flowing to the lungs.
Other types of NIV might include Nasal Intermittent Positive Pressure Ventilation (NIPPV) which uses a ventilator to provide intermittent breaths at full inspiratory pressure through the nose. Bilevel Nasal Positive Airway Pressure (BiPAP) uses lower pressure, longer inspirations and sighs (occasional deeper breaths). These machines follow a typical breathing pattern of taking in air then resting to allow air containing carbon dioxide to flow out.
Mechanical Ventilation
Mechanical Ventilation (MV) is a tube that is placed in the mouth or throat to accommodate breathing. This is considered invasive because the breathing tube is placed inside the body. A tracheostomy, or a surgical incision at the front base of the neck, is made to make the effort of breathing easier if the ventilation will be long term.
There are two basic types of mechanical ventilators:
- Negative pressure ventilators, such as the iron lung, create a vacuum around the outside of the chest, causing the chest to expand and suck air into the lungs.
- Positive pressure ventilators, which have been available since the 1940s, work on the opposite principle, by blowing air directly into the lungs. Ventilators are invasive – an air passage is made in the throat area, fitted with a device most people call a “trach.”
In general, those with complete neurologic injuries at C2 and above have no diaphragmatic function and require a ventilator. Those with complete injuries at C3 or C4 may have diaphragmatic function and may have the potential to be weaned off the ventilator. People with complete injuries at C5 and below have intact diaphragmatic function and may require a ventilator soon after injury but are usually able to wean off the device.
Weaning from mechanical ventilation is important because it reduces the risk of some health issues such as pneumonia and tracheostomy complications. Mechanical ventilatory weaning may result in less paid assisted care.
Settings on the ventilator will be adjusted to your individual needs. Settings should not be adjusted without specific direction. Words that you will hear and should know are:
Peak inspiratory pressure (PIP) is the maximum amount of pressure that the lungs need for inflow of oxygen. This is determined by adequate chest wall movement.
Inspiratory time is the length of time to fill the lungs with air by the machine controlling it.
Positive end expiratory pressure (PEEP) is the pressure in the lungs when air can flow out, or deflated lung pressure. In breathing, air is pulled into the lungs, but the pressure must be relaxed so that air can be allowed to flow out.
PaO2/FiO2 ratio is the ratio of partial pressure arterial oxygen and fraction of inspired oxygen. In other words, this is the amount of oxygen in the lungs that is converted by the alveoli to oxygen in the blood.
Tidal Volume (TV) is the amount of air in and out of the lungs in one breath.
There are a variety of mechanical ventilation adaptors available. Some go through the mouth, but most will have a tracheostomy tube surgically implanted in the neck. This greatly reduces the work of breathing because air does not need to travel through the nose, mouth and throat. Careful hygiene of the area must be performed including tracheostomy tube cleaning and changes to assist in avoiding infection or mucous build up.
There are potential complications related to tracheostomy tubes, including the inability to speak or swallow normally. Speaking loss is one of the most frustrating aspects of mechanical ventilation. Certain tracheostomy tubes are designed to direct air upward during exhalation, and thus permit speech during regular, periodic intervals. Adaptive valves can also be placed to allow speech. These valves can be attached between the tracheostomy tube and ventilatory tubing which will allow the individual to speak on their own. Ventilatory settings are coordinated for speech to occur. Also, computers that can be controlled with eye movement can also be used to speak for the individual.
Another tracheostomy-associated complication is infection. The tube is a foreign body in the neck and thus has the potential of introducing organisms that would ordinarily be stopped by natural defense mechanisms in the nose and mouth. Cleaning and dressing the tracheostomy site daily is an important preventive measure.
Suctioning is typical with ventilatory support to clean the lungs from excessive mucous and secretion build up. Suctioning requires sterile technique. A new, sterile suction catheter is used at each suctioning session. It can be entered and exited several times in one suctioning event but never saved for later use due to bacteria build up. A suction catheter should be appropriate for the size of the patient and the tracheostomy.
The suction catheter should be moving the entire time it is inside the airway. Allowing the suction to rest against the delicate airway tissue can lead to bruising or bleeding. Suction is off when entering the airway and on when removing the suction catheter. The time the suction catheter can be in the lungs should not surpass the amount of time you can hold your breath. If there is difficulty in entering each lung and the individual does not have spinal precautions, have the individual turn their head slightly to the opposite direction of the lung to be suctioned. This adjusts the internal physiology of the body so suctioning of each lung becomes easier.
Most individuals find suctioning to be uncomfortable but tolerable. If suctioning is an issue, you might want to consider a CoughAssist (insufflator) as an alternative for cleaning the airway as it is a bit more gentle although it can take some time to become used to it.
There are several machines on the market to promote coughing for individuals who are dependent on ventilators:
The Vest consists of an inflatable vest connected by air hoses to an air pulse generator, which can rapidly inflate and deflate. This applies gentle pressure to the chest wall to loosen and thin mucus and move it to the central airways to be cleared by coughing or suctioning.
CoughAssist machines, as mentioned above, are designed to boost cough function by mechanically simulating the cough maneuver. This device blows in an inspiratory pressure breath followed rapidly by an expiratory flow.
* Both the Vest and the CoughAssist have been approved by Medicare for reimbursement if determined to be a medical necessity.
Respiratory Implants (Neuroprosthesis)
A Phrenic Nerve Pacemaker is an implant that is placed on the diaphragm in a minimally invasive surgical procedure. A control is placed on the outside of the body that provides an electrical stimulation to the phrenic nerve to cause it to contract. Phrenic nerve pacers have been available for several years. Two companies offer diaphragm stimulation systems:
The Avery pacemaker has been in use since before the FDA approved medical devices, going back to the mid-1960s. The procedure involves surgery through the body or neck to locate the phrenic nerve on both sides of the body. The nerves are exposed and sutured to electrodes. A small radio receiver is also implanted in the chest cavity; this is activated by an external antenna taped to the body.
The Synapse system, pioneered in Cleveland, was used in an early clinical trial by Christopher Reeve in 2003. The Cleveland system, FDA approved for implant in people with spinal cord injury in 2008, is more simply installed, using an outpatient laparoscopic technique. Two electrodes are placed on each side of diaphragm muscle, with wires attached through the skin to a battery powered stimulator. Synapse also has FDA approval to implant the devices in people with ALS.
Researchers at the Cleveland FES Center have devised an electrical stimulation protocol to initiate a forceful cough in tetraplegic patients, on demand. The system is under evaluation and not yet clinically available.
Rehabilitation
A physiatrist or specialist in physical rehabilitation will lead your care for all your spinal cord injury needs. Basic and advanced respiratory assessments will be made with consults to pulmonary specialists as needed.
Pulmonary (breathing) specialists direct the care of individuals with respiratory issues. The pulmonary specialist is most often consulted if you have multiple respiratory conditions or need advanced respiratory care.
An Interventional Radiologist may work with your pulmonary specialist to perform tests of your respiratory function of if you have a respiratory implant or neuroprosthesis for breathing.
The Respiratory Therapist (RT) is going to be an important member of the team if you have respiratory difficulty. This specialty consists of specially educated individuals who will monitor, administer medication and treatment for your breathing issues. You may receive a variety of treatments specialized to your needs from the RT. These treatments can include care of your mechanical ventilation to home care exercises to improve your breathing ability.
Rehabiliation nurses are instrumental in detecting breathing issues, providing treatments and medications that will assist with your respiratory health as indicated by your physiatrist, pulmonologist and respiratory therapist. The nurse will care for your needs in the ICU, rehabiliation hospital and may be a part of your home care team.
Physical Therapy (PT) will be provided to assist you with motor skills to adapt to your breathing needs. They will teach you to conserve energy if needed as well as how to strengthen your muscles for breathing.
Occupational Therapy (OT) provides education and treatment for activities of daily living that may need to be altered due to your breathing status as well as how to adapt activities with breathing assistance devices.
The Speech/Language Pathologist (SLP CCC) will assist you with learning to speak and swallow with adaptive breathing devices as well as how to decrease your risks of choking (aspiration).
A Psychologist will provide mental health assistance in learning to adjust to your new way of living.
The Social Worker will assist you and your family with locating resources and staff to assist you at home.
An Insurance Case Manager can assist with locating the care providers and equipment needed for your health status.
Research
Both bench (laboratory) and clinical (with people) research studies into effective breathing function abound. Research concerning the respiratory system crosses all medical disciplines. What is discovered for one diagnosis is used in other diagnoses resulting in a wide sharing of knowledge.
To improve breathing for individuals with any issue in the respiratory system, advances in technology have been and continue to occur. The number and type of devices available have greatly increased options in the recent past. People are looking toward more effective, more comfortable and easier to use devices and parts.
Research specifically for individuals with spinal cord injury consists of understanding how the respiratory nerves work with the long-term goal of improving breathing. Many researchers are studying how the respiratory system develops in the fetus to see if that natural development can be harnessed and used for treatment of respiratory issues after spinal cord injury. In the fetus many nerves are developed to make the phrenic nerve. Those nerves that are extra are naturally eliminated prior to birth. Stimulation of the development of extra phrenic nerves may be one source to improve breathing after SCI.
The neurological phenomenon of plasticity is being used. Plasticity is the theory that the nervous system will adapt to challenges. This theory is used through all SCI and neurological research. Researchers are interested in learning how the nervous system will adapt to SCI and how this process can be prompted and enhanced.
Exercises to improve breathing are taught to individuals with SCI at all levels. Studies are being conducted to establish which are the most effective and at what level of injury. There appears to be some natural recovery of the respiratory system within the first year of injury. How this improvement occurs and how it can be used to further improvement is being researched.
Medications that assist breathing continue to be researched. One example is Theophylline, a medication that is used in respiratory conditions such as asthma, which is also used and studied for individuals with SCI. Also, muscle relaxant medication for spasticity is under study to find the balance and best route of administration to reduce spasticity without reducing the ability to breathe.
Respiratory SCI Facts and Figures
80% of individuals with spinal cord injury from disease or trauma will be affected by respiratory complications. *
The most common respiratory complications after SCI are atelectasis (partial or total lung collapse), pneumonia (bacterial, viral or fungal infection) and respiratory failure (inability to bring oxygen into the body and/or release carbon dioxide).*
One study found respiratory complications in individuals with C1-C4 injury to be 84%, C5-C8 60% and T1-T12 65%.**
Consumer Resources
If you are looking for more information about Respiratory Management after SCI or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm ET.
Additionally, the Reeve Foundation maintains fact sheets with additional resources from trusted Reeve Foundation sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to spinal cord injury support groups and organizations, including:
PVA Consortium for Spinal Cord Medicine Clinical Practice Guidelines. (2005). Respiratory Management Following Spinal Cord Injury: A Clinical Practice Guideline for Health-Care Professionals. Paralyzed Veterans of America. www.pva.org
American Lung Association Support Groups
Further Reading
References
Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe (Sheff). 2016 Dec; 12(4): 328–340. doi: 10.1183/20734735.012616 PMCID: PMC5335574 PMID: 28270863
Brown R, DiMarco AF, Hoit JD, Garshick E. Respiratory Dysfunction and Management in Spinal Cord Injury. Respir Care. 2006 Aug; 51(8): 853–870. PMCID: PMC2495152 NIHMSID: NIHMS43993 PMID: 16867197
Cardozo CP. Respiratory Complications of Spinal Cord Injury. J Spinal Cord Med. 2007; 30(4): 307–308. doi: 10.1080/10790268.2007.11753945 PMCID: PMC2031931 PMID: 17853651
Goshgarian HG. The crossed phrenic phenomenon: a model for plasticity in the respiratory pathways following spinal cord injury J Appl Physiol (1985). 2003 Feb;94(2):795-810. doi: 0.1152/japplphysiol.00847.2002. PMID: 12531916 DOI: 10.1152/japplphysiol.00847.2002
Hristara-Papadopoulou A, Tsanakas J, Diomou G, Papadopoulou O. Current devices of respiratory physiotherapy. Hippokratia. 2008;12(4):211-20. PMID: 19158964
**Jackson AB, Groomes TE. ©1994 by the American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and Rehabilitation. Incidence of Respiratory Complications Following Spinal Cord Injury. Arch Phys Med Rehabil Vol75, March 1994. https://www.archives-pmr.org/article/0003-9993(94)90027-2/pdf
National Spinal Cord Injury Statistical Center. Spinal Cord Injury Facts and Figures at a Glance. 2019. https://www.christopherreeve.org/wp-content/uploads/2024/04/Facts20and20Figures20201920-20Final.pdf
Ozpinar A, Weiner GM, Ducruet AF. Epidemiology, clinical presentation, diagnostic evaluation, and prognosis of spinal arteriovenous malformations. Handb Clin Neurol. 2017;143:145-152. doi: 10.1016/B978-0-444-63640-9.00014-X.PMID: 28552136 DOI: 10.1016/B978-0-444-63640-9.00014-X
Schilero GJ, Spungen AM, Bauman WA, Radulovic M, Lesser M. Pulmonary function and spinal cord injury. Respir Physiol Neurobiol. 2009 May 15;166(3):129-41. doi: 10.1016/j.resp.2009.04.002. Epub 2009 Apr 9.
Slack RS, Shucart W. Respiratory dysfunction associated with traumatic injury to the central nervous system. Clin Chest Med. 1994 Dec;15(4):739-49.
*Tollefsen E, Fondenes, O. Respiratory complications associated with spinal cord injury. Tidsskr Nor Legeforen 2012, 132: 1111. doi: 10.4045/tidsskr.10.0922
Zimmer MB, Nantwi K, Goshgarian HG. Effect of Spinal Cord Injury on the Respiratory System: Basic Research and Current Clinical Treatment Options. J Spinal Cord Med. 2007; 30(4): 319–330. doi: 10.1080/10790268.2007.11753947 PMCID: PMC2031930 PMID: 17853653