Spinal Cord Injury
Spinal cord injury occurs when something interferes with the function or structure of the cord. This can include consequences of a medical illness or trauma resulting in over stretching the nerves, a bump, the bone of the vertebra pressing against the cord, a shock wave, electrocution, tumors, infection, poison, lack of oxygen (ischemia), cutting or tearing of the nerves. Spinal cord injury can occur as a fetus develops, from trauma or medical conditions.
Results of a spinal cord injury can appear differently depending on the type and location of the injury. The most common is loss of motor, sensory and slowing of some of the body’s internal organs (autonomic nerve function) below the level of the injury. In general, the higher in the spinal cord an injury occurs, the more function, sensation and internal body functions will be affected.
Injury that affects all four limbs is called tetraplegia (this used to be called quadriplegia). An injury that affects the lower half of the body is called paraplegia. The significance of these injuries is much more than just arm and leg movement as sensation and all body systems are affected.
Complete injuries are those where there is no function or sensation below the level of injury. It really means all messages to and from the brain are completely blocked. It does NOT mean your spinal cord is completely severed. Complete injuries indicate no messages are getting through the affected area of injury in the spinal cord. Incomplete injury indicates some messages are getting through. Incomplete injuries are unique to the person. No two incomplete injuries are exactly the same, although they can be similar. Abilities of an individual with an incomplete injury depend on which nerves are transmitting messages.
Individuals with spinal cord injury from medical causes might have several locations of injury resulting in mixed results. Disease caused spinal cord injury evolves over time as the medical condition progresses. An individual may be able to compensate for some muscle weakness or sensory loss in the early stages of the disease. However, at some point, a critical level of disease will occur where function or sensation is severely diminished or lost. No one knows exactly when this time will occur as it is individual for everyone by type of disease and progression.
Traumatic injury occurs suddenly, mostly due to an accident. The area of the spinal cord involvement might be at one level or consecutive levels. Some people might have trauma at two different level of the spinal cord or more depending on location(s) of the injury. Other trauma to the body may also occur at the same time. Effects of the spinal cord injury is immediate.
Medical professionals might use the term ‘lesion’ to describe the sight of a spinal cord injury. A lesion is damage to an area of the body. It can be from trauma, bruising, pressure, tumor, lack of oxygen, scarring, plaque or any cause of disruption to the spinal cord.
An injury in the cervical and thoracic area of the spinal cord results in an upper motor neuron lesion (UMN). This type of injury is associated with the development of tone (spasticity). You will see this in your muscles of your arms and legs perhaps even in your trunk. Inside your body, organs are also affected by tone. Tone is easiest to notice internally by bowel and bladder function as small amounts of stool or urine automatically being expelled without emptying.
In the lumbar and sacral areas of the bowel, a lower motor neuron lesion (LMN) occurs. This injury results in flaccidity. Very soon after your injury, you might notice the muscles of your legs becoming smaller as the muscles lack tone. The bowel and bladder will fill but not expel stool or urine. Both can become overdistended leading to major complications. Sometimes, the bowel and bladder will expel overflow waste without emptying.
Other Types of Spinal Cord Injury
There are other less common types of spinal cord injury that affect specific areas of the spinal cord.
Anterior Cord Syndrome (sometimes called Ventral Cord Syndrome) is caused by lack of blood flow or lack of oxygen (infarction) to the front two thirds but not the back of the spinal cord and in a part of the brain called the medulla oblongata. The result is loss of motor, pain and temperature sensations but where your body is in space (proprioception) and vibration sensations remain from the level of injury down. Individuals with Anterior Cord Syndrome will note their body position by visually observing their environment as opposed to sensing where their body is positioned.
Central Cord Syndrome is usually caused most often by a fall with over stretching (hyperextension) of the neck. Loss of function occurs from the neck to the nipple line which includes the arms and hands. The torso has variable function and sensation. The lower body has unaffected function but variable to total lack of sensation. Individuals with this type of injury usually retain the ability to walk but might have poor balance. Central Cord Syndrome occurs most often in elderly individuals due to decreased flexibility with age.
Posterior Cord Syndrome results in loss of light touch, vibration and position sense starting at the level of injury. Motor function remains. It is caused from trauma, compression of any length of the back side of the spinal cord, tumors and Multiple Sclerosis.
Brown-Séquard Syndrome is noted by one side of the body with motor function loss and the other side of the body with sensation loss. Depending on the location of the injury, the result can be presented as tetraplegia or paraplegia. Brown Sequard Syndrome can be caused from a tumor, injury, ischemia (loss of oxygen), puncture, infection or Multiple Sclerosis (MS).
Cauda Equina is an injury to the nerve roots below L2 which results in leg weakness, bowel incontinence, urinary retention and sexual dysfunction.
Conus Medullaris can be caused from an injury or disease affecting the core of nerves inside the nerve root. Injury to this area results in an incomplete spinal cord injury affecting leg function, bowel, bladder and sexual function. Pain is typically present.
Cord Concussion results from a bump to the spinal cord. Much like a concussion to the brain, the spinal cord can be bruised or have message disruption for about 48 hours with possible return of function thereafter. As with brain concussion, long term dysfunction of various types can occur. Cord concussion is sometimes referred to as a ‘stinger’ especially in the sporting world.
Tethered Cord is an attachment of the spinal cord to the tissues in the tract where the spinal cord is housed in the body. This typically is an anatomical anomaly formed as a fetus and not detected until birth or later in early childhood. Sometime, tethered cord is not detected until adulthood. Surgery can release the cord if necessary. Tethered cord can appear after spinal cord injury due to complications of the injury.
Spina Bifida and other neural tube diseases occur in fetal development. The spinal cord does not form in the enclosed space of the vertebrae. In utero surgery (surgery before birth) can possibly correct spinal placement before a baby is born. Surgery after birth can correct the placement but with mixed results. Taking folic acid (vitamin B9) during pregnancy can reduce the risk of spina bifida. A vitamin like molecule, Inositol, is being tested to assess if prevention of neural tube defects is possible.
Body Areas Controlled by Spinal Cord Sections
Note: sensation is affected from the level of injury and below.
Cervical Spinal Cord Section
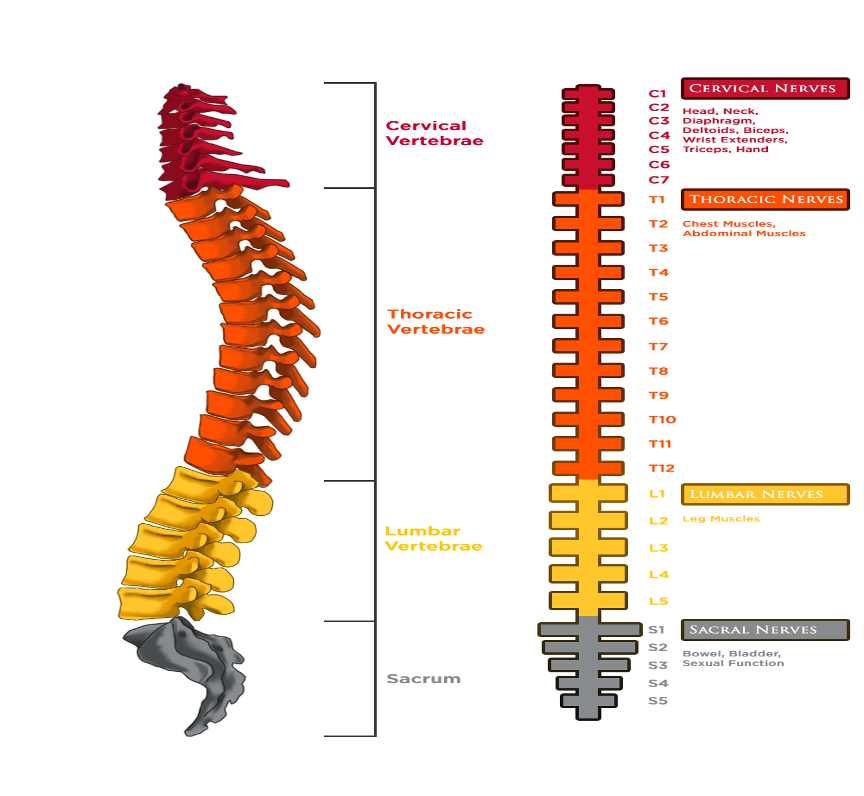
The nerves exiting the vertebrae in the neck area or cervical segments are referred to as C1 through C8. These nerve control signals to the neck, arms, hands, and internal organs. Injuries to these areas result in tetraplegia. Injuries at the cervical level can distort where your body is positioned in space (proprioception.)
An injury above the C3 level may require a ventilator for breathing.
Individuals who have an injury above the C4 level usually means loss of movement and sensation in all four limbs, although often shoulder and neck movement is available to facilitate sip and puff devices for mobility, environmental control and communication.
Individuals with C5 injuries often have control of shoulder and biceps, but there is not much control at the wrist or hand. Individuals with a C5 level of injury typically can feed themselves and perform some activities of daily living.
An individual with an injury at C6 generally has enough wrist control to be able to drive adapted vehicles and handle some toileting activities but lack fine motor control.
Thoracic Spinal Cord Section
Nerves in the thoracic or rib cage area (T1 through T 12) relay signals to the torso and some parts of the arms.
Individuals with injuries from T1 to T8 usually affect control of the upper torso, limiting trunk movement and sensation as the result of a lack of abdominal muscle control. This can affect balance as well as proprioception (where your body is in space).
Those individuals with lower thoracic injuries (T9 through T12) have trunk control and some abdominal muscle control.
Lumbar and Sacral Sections
Nerves in the lumbar and sacral levels of the spinal cord affect the legs, bowel, bladder and sexual function. The lower nerves are peripheral nerves (outside of the spinal cord) and might be able to be transferred, split or grafted surgically to improve function.
- Individuals with injuries in the lumbar or mid-back area just below the ribs (L1-L5) affect messages to and from the brain to the hips and part of the legs.
- A person with an L4 injury can often extend their knees.
- The sacral sections (S1 through S5) lie just below the lumbar segments in the mid-back and control signals to the groin, toes, and some parts of the legs.
- Bowel, bladder and sexual function is affected.
- The spinal cord is numbered by the boney vertebrae that houses it. You will notice that the bones that surround the spinal cord are not stacked directly on top of each other but have some gentle curves to allow movement in the back and torso. The nerves of the cervical (C) spinal cord are numbered from 1-8. C1 is located in the skull, C2-C8 are located in the neck. Thoracic (T) vertebrae are the back bones that have ribs attached. Thoracic vertebrae are numbered T1-T12. Lumbar (L) spinal cord segments are at the small of the back and number L1-L5. The sacral (S) spinal cord segments are the last of the spinal cord nerves in the ‘shield’ looking shaped tail bone. Sacral nerves are S1-S5. There is one coccygeal segment.
- The spinal cord consists of a bundle of nerves that travel down the back from the brain through the back bones or vertebrae. The nerves of the spinal cord and the bones that protect the spinal cord have the same section (cervical, thoracic, lumbar, sacral) and number notation. Each vertebra has two nerves that exit from either side that control a segment of the body called a dermatome. Each nerve controls the function, sensation and autonomic nerves of that part of the body.
- The nerves that exit the spinal cord are specific to each area of the body. This is how you and your healthcare providers will communicate function and sensation. Key levels include C3 and above which, if injured, will require mechanical ventilation for breathing. In the cervical levels, your function and sensation are tetraplegic (the same as quadriplegic) or involving all four limbs. Paraplegia is diagnosed at T1, which means arm and hand function is intact, but trunk and legs have limitations. Individuals who have sacral level injury will be able to walk with assistive devices but will have limitations in bowel, bladder and sexual function.
- It is a bit difficult to locate some levels of the spinal cord on the body especially in the trunk where there are no particular differentiation points. T4 is at the nipple line. T10 is at the umbilicus or belly button. If you start at T4 and count down by two finger widths you will be at T5, two more consecutive finger widths downward is T6. Keep going and you will end up at the umbilicus or belly button which is T10.
Understanding the Spinal Cord-Physiology
There are two main parts of the nervous system, the central nervous system (CNS) and the peripheral nervous system (PNS). The central nervous system (CNS) is made up of the brain and spinal cord which is the nerve center of the body. The brain creates, interprets and responds instantly to messages sent to and from the body by way of the spinal cord. Without this unit of communication, the nerves in the body, called the peripheral nervous system (PNS), cannot report to the brain or respond with actions or feel sensations.
A nerve cell is called a neuron which consists of a cell body with many branch-like projections called dendrites. There is one long projection from the cell body called an axon. Axons carry messages away from the cell body. Axons in the spinal cord carry signals downward from the brain (along descending pathways) and upward toward the brain (along ascending pathways.)
Nerve cells of the CNS have a very high rate of metabolism and rely upon blood glucose for energy – these cells require a full blood supply for healthy functioning; therefore, CNS cells are particularly vulnerable to reductions in blood flow (ischemia). Other unique features of the CNS are the “blood-brain-barrier” and the “blood-spinal-cord barrier.” These barriers, formed by cells lining blood vessels in the CNS, protect nerve cells by restricting entry of potentially harmful substances and cells of the immune system. Trauma may compromise these barriers, potentially contributing to further damage in the brain and spinal cord. The blood-spinal-cord barrier also prevents entry of some therapeutic drugs.
Cells that Control Spinal Cord Function
Several types of cells carry out spinal cord functions, including:
- Long axons that control skeletal muscles in the neck, torso, and limbs are called large motor neurons.
- Sensory neurons called dorsal root ganglion cells, or afferents, carry information from the body into the spinal cord and are found immediately outside the spinal cord.
- Cells that help integrate sensory information and generate coordinated signals that control muscles are called spinal interneurons. These cells lie completely within the spinal cord.
- Supporting cells (called glia), far outnumber neurons in the brain and spinal cord and perform many essential functions. Glial cells produce substances that support neuron survival and influence axon growth. However, these cells may also impede recovery following injury; some glial cells become reactive and thereby contribute to formation of growth-blocking scar tissue after injury.
- Creating the myelin sheaths that insulate axons and improve the speed and reliability of nerve signal transmission is a specific type of glial cell called the oligodendrocyte.
- Large star-shaped glial cells regulate the composition of the fluids that surround nerve cells. Some of these cells named Astrocytes, also form scar tissue after injury.
- Smaller cells become activated in response to injury and help clean up waste products. These cells are called microglia.
In the spinal cord, the outer most nerves are coated with myelin, a white, fatty, segmented substance produced by oligodendrocytes and Schwann cells. Where axons are coated with myelin is called white matter. Inner spinal cord nerves are not coated with myelin, so they are called gray matter. The gray matter nerves are in the center of the spinal cord, in a butterfly shape. Peripheral nerves, those in the body, are all myelinated.
Sending messages between the brain and body takes a complicated system of nerves. There are three specific types of neurons that work to accomplish this function. Sensory impulses from all parts of the body are transmitted by nerves called afferent neurons. Movement messages sent from the brain through the spinal cord with the signal to move the body are transmitted by motor neurons. Together, sensory neurons and motor neurons send messages through complexly formed networks of nerve fibers called interneurons, also called central or connecting neurons.
The brain and the spinal cord are the consistency of very thick gelatin. The diameter of spinal cord is about the size around your thumb. It is about 18 inches long. Both the brain and spinal cord are surrounded by cerebral spinal fluid to cushion and protect the delicate nerve tissue. The bones of the skull protect the brain. Vertebrae bones protect the spinal cord. Nerve roots exit both sides of each segment of the spinal cord. The spinal cord ends at level L1 (first vertebrae at the lumbar level) or at the small of your back. The rest of the vertebrae carry nerve roots that also exit on both sides of the lower vertebrae.
The spinal cord is enclosed within three membranes (meninges). These enclosures are the same as in the brain. You might hear these words discussed, especially if you are having or had surgery to the area around the injury of your spinal cord:
- Pia mater: inner most layer
- Arachnoid: delicate middle layer
- Dura mater: tougher outer layer
Diagnosing Spinal Cord Injury
Imaging using MRI or CT scans will provide information about a spinal cord injury including the type and level where the trauma occurred. This might not match up to your clinical exam as the injury could be at one level, but your level of function might indicate a higher level of injury due to swelling and other trauma or medical complications. To evaluate the functional outcomes of spinal cord injury, a physical examination is performed.
Spinal cord injury is evaluated using the International Standards for Neurological Classification of SCI (ISNCSCI). The same scale should be used to assess your spinal cord injury each time to be able to track your progress accurately.
Each level of the spinal cord is tested by assessing the dermatome or specific body section affected by the nerve at each level of the cord. In testing, motor ability is assessed by moving every joint in your body. Assessments are made to see if you can move under your own power, positioned so gravity is reduced, or unable to move. Sensation is assessed for gross and fine sensation. Both gross sensation, measured using a cotton swab, and fine motor sensation, measured using a sharp point, are tested. Sensation is measured by full feeling, feeling present but feels different and no feeling.
Using the International Standards for Neurological Classification of SCI (ISNCSCI) by a certified professional, the last fully functioning nerve becomes your level of injury. This might be the same on both sides of the body but since there is a nerve exiting the side of each vertebrae, occasionally, there is some slight difference between sides of the body. An example would be T4 on the right and T6 on the left side of your body.
Sometimes, there can be some partial function of nerves below the last fully functioning segment and nerves with a lack of function. This is indicated as a zone of partial preservation (ZPP). An example would be a spinal cord injury level of T8 with a ZPP T12 meaning T8 is the last fully functioning spinal nerve but there is some function in the nerves of T9 through T12. These nerve preservations might not be noted in your diagnosed level because it is the last fully functioning nerve the one that is documented.
Levels of injury are assigned to indicate impairment. This is a method of communication for healthcare professionals to understand the extent of injury. The ASIA Impairment Scale (AIS) from the American Spinal Injury Association is available on the International Standards for Neurological Classification of SCI (ISNCSCI) Worksheet. The AIS uses the following 5 categories (A-E); please see the link above for their definitions.
A. Complete injury. This means no function or sensation is assessed at the end of the spinal cord.
B. Sensory incomplete. This level indicates sensory but not motor function is retained and no motor function is present within three levels of injury on either side.
C. Motor incomplete. Motor function is present to the end of the spinal cord.
D. Motor incomplete. Muscle function below level of injury is against gravity.
E. Normal. No residual affects assessed.
A complete injury is often confused with a completely transected cord. The designation of complete injury means a complete interruption of messages through to the last nerve of the spinal cord. Rarely is the spinal cord completely severed. Complete severing might occur if a knife or bullet passes directly through the center of the spinal cord. In complete spinal cord injury, there are typically nerve fibers that are still attached that may or may not be transmitting messages.
Treatment for Spinal Cord Injury
Immediately after a spinal cord injury, the individual is placed on a back board with a neck brace to help stabilize the spine. No one should move the individual unless they are proficient with the precautions that will protect the spine from further injury. Spinal cord injury can be life threatening, requiring emergency treatment.
In the emergency room, two of the first tests will be an MRI or CT scan to check the image of the spine and a physical examination. The results of these tests will direct treatment. If your spinal cord is unstable, meaning that the boney vertebrae are unable to protect it, surgery might be immediately performed to create the stabilization. Surgery will most often consist of rods or plates to hold the bones together. If there are other injuries or medical issues, the spine surgery may be delayed until your life is stabilized.
After surgery, typically is a stay in the intensive care unit (ICU) where rehabilitation therapy will continue at an appropriate level. This will consist of movement applied to the body and safety prevention measures. There might also be some functional electrical stimulation (FES) to provide input to the nerves and muscles below the level of injury. Adaptive equipment will be provided to maintain skin, bowel and bladder function.
From the ICU, the individual will be moved to an inpatient nursing unit or directly to a rehabilitation facility where recovery will continue. Advancements in treatment are made with improvement which can either be with improvement within your body or improvement by use of adaptive equipment.
Transition to home or the location where you will live is the next step. Rehabilitation will continue through outpatient treatment, home therapy or an independent therapy program. Lifelong therapy is needed to maintain your function and continue improving. It might be that you will need to continue therapy on your own, without a therapist present, but keeping up with activity is important to your lifelong treatment.
The nervous system has been determined to be plastic, meaning it will adapt to changes within it. Keeping yourself healthy is significant to improving function and being ready for future therapies as they become available.
Recovery from Spinal Cord Injury
Recovery from spinal cord injury can be a slow process. The body’s normal defense mechanism when injured is to rush fluid to the area to provide an extra cushion and to send white blood cells to remove any foreign substances. This is how the body naturally cares for itself. However, there is no room in the boney casement of the vertebrae, so this extra fluid will push on viable tissue which can restrict blood flow. Controlling for edema will be imperative to treatment to avoid additional damage to your injury site.
Unique to the central nervous system is a process called apoptosis or programmed cell death. To help the body cope with the extra fluid pumped into an injured area when a nerve cell is damaged, other cells die as the body attempts to control for too much substance in the vertebral column. This is the body’s way of saving itself but in doing so, more nerves can be destroyed.
The good news is that after swelling and apoptosis slows, there will be less pressure on your nerves. You might see some improvement in function, perhaps even an improvement in functional level by a nerve segment or two.
Secondary Conditions Due to Spinal Cord Injury
Besides a loss of sensation or motor function, injury to the spinal cord leads to other changes in the body. Your body is still working below the level of injury. It is just that messages to and from your brain are not being communicated through the site of injury. You will have to provide your body with the necessary care manually. Complications of spinal cord injury are possibly preventable with good healthcare, diet and physical activity although sometimes they occur even with the best of intentions. The chart below indicates the secondary complications of spinal cord injury and ideas about how to combat them.
| Body System | Secondary Complication | Paralysis Effects | Suggestions for Treatment |
|---|---|---|---|
| Musculoskeletal | Calcium loss | Calcium loss from lack of movement through long bones of the legs, fractures | Keep track of bone density though regular bone density testing and treat as recommended by your healthcare professional.Use of a standing frame (with gliders if able to use) to put movement through the legs. |
| Heterotrophic Ossification (H.O.) | Overgrowth of bone into soft tissue (muscle) | Perform range of motion exercise to joint to keep them pliable.Medication: etidronate disodium (Didronel) to reduce bone growth.Surgical removal. | |
| Loss of muscle tissue | Replacement of muscle with fat, stomach pouch, scoliosis, skin breakdown | Exercise as able. Move all body joints several times a day. Use resistance bands if possibleSome drugs can decrease muscle tone but have significant side effects, discuss with healthcare professional when appropriate. | |
| Upper extremity pain | Shoulder pain from propelling wheelchair, rotator cuff injury, bursitis, capsulitis | Work with therapist to learn techniques for strengthening.Don’t reach back so far to propel manual wheelchair.Add power assist to your wheels | |
| Poor muscle tone | Scoliosis or curvature of the back | Strengthening exercises for the back.Sit up, use excellent posture.Utilize positioning equipment when sitting or lying. Monitor equipment for wear and damage. | |
| Tone (spasticity) | Spasms of muscles of the extremities and inside the body in individuals with cervical and thoracic injuries. Can be painful or prevent correct positioning of body. | Move and stretch muscles frequently during the day. Fatiguing the muscle can reduce tone.Use medication as needed to reduce tone and pain, if necessary.Some tone can be effective for assisting with transfers.
Use advanced therapies to exercise muscles to reduce tone. |
|
| Flaccidity | Lack of muscle tone in the lower extremities and the body in lumbar and sacral injuries. | Provide manual movement to the lower extremities to keep muscles pliable. | |
| Nervous | Slowing rate of information processing | Complicated by injury to the brain | Exercise your brain as well as your body. Examples: play word and math games, expand hobbies or new interests.Engage in conversation and socialization. |
| Decreased balance and coordination | Spasticity | Stretching for all parts of your body on a regular basis. | |
| Muscular pain and Neuropathic pain | Nerve pain from inefficient nerve transmissions | Discuss option with your healthcare specialists for non-narcotic treatment options.Exercise and stretch muscles which fatigues them making spasms less frequent and less severe. | |
| Depression | Due to chronic illness/disability | Discuss your mental health with a professional for a checkup and/or treatment.Become active in the SCI community to exchange ideas and opportunities. | |
| Cardiovascular | Autonomic Dysreflexia (A.D.) | Misinterpretation of nerve impulses | Know the warning signs and treatments. https://www.christopherreeve.org/living-with-paralysis/free-resources-and-downloads/wallet-cards |
| Orthostatic hypotension-low blood pressure, fainting | Poor return of blood through the veins | Keep up with drinking fluids.Use elastic blood return flow garments especially full leg and abdomen. | |
| Deep Vein Thrombosis (DVT)Pulmonary Embolis (PE) | Pressure on blood vessels from external forcesPoor circulation | Don’t cross your legs or ‘hook’ your arm.Wear prevention elastic stocking on legs or arms.Use blood thinning medication, only if prescribed. | |
| Edema | Poor return of fluid from the legs and arms | Elevate affected body part higher than the heart.Use elastic blood return flow garments.Diuretic medication if indicated. | |
| Exercise intolerance | Ineffective distribution of oxygen in the blood | If unable to perform the exercise routine that you did earlier, modify but stick with a plan. | |
| Increased cardiac risk | Develops over time. | Control factors such as diet, exercise, weight gain, cholesterol, blood pressure | |
| Respiratory | Decreased lung capacity | Restriction of breathing, poor posture | Breathe in deeply and exhale completely at regular intervals throughout the day.Cough.Strengthen chest muscles with therapy. |
| Pneumonia | Infection in the lungs | Deep breath and cough to keep passages clear.Keep mouth clean to avoid aspiration of food particles.Suction as needed.
Antibiotics for infection. |
|
| Mechanical Ventilation | In individuals with injury above C3 | Use mechanical ventilation as required.Strengthen muscles through respiratory therapy.Suction as needed or opt for an insufflator. | |
| Gastric | Slower bowel absorption, Neurogenic bowel | Slowing bowel leading to constipation, enlarged colon, hemorrhoids, colorectal cancer | Increase roughage in your diet through food or bulk formers.Use stool softener as needed.Very slowly, increase fluid.
Generous use of lubricant during bowel program. With spastic bowel (cervical and thoracic injuries) performs digital stimulation slowly to relax sphincter. |
| Changes in ability to control cholesterol | Low HDL-good cholesterol | Use medication as prescribed.Exercise either actively or passively. | |
| Urinary | Kidney stones | Less ability to filter urine | Know your body so you can report a change to recognize there might be a problem, so this diagnosis can be made without delay. |
| Neurogenic Bladder | Failure to empty bladder at the appropriate time | Management with intermittent bladder catheterization, external catheter for men, indwelling catheter, suprapubic catheter, Mitrofanoff procedure or a combination of methods depending on individual needs. | |
| Urinary Tract Infection (UTI) | Bacteria in urine | Maintain hydration.Remove soap residual or sanitizer after catheterization.Liberal use of lubricant.
Maintain hygiene of bladder opening and hands. Antibiotics as needed. |
|
| Endocrine | Low testosterone | Reduction in hormones | Discuss treatment options with your healthcare provider to see if you want treatment for this condition. |
| Higher incidence of Type II Diabetes | Decreased metabolism of insulin | Perform exercises as you are able either actively or passively.Medication as necessary. | |
| Immune | Slowing of the immune system reactions | Increased chance of infection | Wash your hands frequently.Use strict cleanliness with catheterizations.Avoid individuals with respiratory infections. |
| Septicemia | A massive infection that affects key body organs. | Follow up with treatment for any infection to avoid spreading.Know the signs and symptoms for sepsis medical emergency:https://www.christopherreeve.org/living-with-paralysis/free-resources-and-downloads/wallet-cards | |
| Skin | Increase in skin breakdown or pressure injury | Decreased elasticity, pressure from bones, lack of movement | Perform pressure releases.Skin checks. Know what your skin looks like. |
| Groin rash | From moisture in damp, closed areas. | Frequent hygiene.Air groin area daily.Apply rash protection when needed. | |
| Nail care | Fragile nails or nail fungus | Maintain hygiene.Trim nails carefully to avoid cuts.Allow air to circulate to toes with natural fiber socks and shoes. | |
| Dry skin and callouses | Immobility | Gently and slowly remove skin with dry washcloth for friction.Apply lanolin moisturizer.Maintain hydration. | |
| Digestive | Lower calorie needs | Obesity, stomach pouch | Follow a nutritious but portion-controlled diet. |
| Feeling full all the time | Slowing moving bowel | Increase fiberEat small portions but at closer intervals. | |
| Reproductive | Sexual dysfunction | Erectile dysfunction in males, lubrication dysfunction in females | Males have options of erectile dysfunction medication, penile injections and implants.Some females respond with Viagra.Both might need to alter sexual function with different positions and strategies. |
Rehabilitation
Activity
Activity is the best way to keep your body healthy and to avoid complications. Research has demonstrated the benefits of activity in maintaining health and function as well as recovery. The body is always attempting to repair itself. Sometimes individuals feel that if they cannot obtain some of the advanced equipment, that the door for recovery is closed. This is far from true. Any type of activity provided to the parts of your body affected by paralysis will help you maintain your body.
Performing range of motion exercises either by yourself or by someone else moving your body will help to keep your joints supple and will assist with bowel, bladder and skin care. Movement of the legs and trunk keep your bowels moving and the urine in your bladder stirred, thereby reducing your chances of infection. Moving your body by performing pressure releases keeps small blood vessels from collapsing or clotting.
When moving affected parts of your body, be gentle. Sometimes when people have decreased sensation, it is easy to throw body parts around. This can include tossing a leg up on the bed or flipping a body part from one spot to another. Range of motion can become harmful when caution is not used. A body part can hit up against the wheelchair, bed or wall. People who have sensation have a natural protection mechanism because humans do not like to cause pain to themselves. With decreased sensation, you need to use caution to keep from harming yourself as evidenced by bruising or even bone fractures. Rough handling can lead to joint problems and deep vein thrombosis or blood clots.
Sometimes, you can find therapies in the least expected places. There might be a therapist in your town that will provide therapy at a reduced rate. Another option is using the local gym with a personal trainer who has experience with individuals with paralysis. Some rehabilitation centers open their gyms in the evening hours for a nominal fee.
Finding activity options can take a lot of effort. If you are active in a community with individuals who have paralysis, you can get some good leads from your friends. The peer support center at the Christopher & Dana Reeve Foundation’s National Paralysis Resource Center can put you in touch with others in your community that might have the information you need, or you can divide the work with them to find or even organize something in your area.
People often overlook aquatic therapy for activity. Many local Y’s have pools that can be heated and personnel who have education for working with individuals with special needs. Some community centers also offer these resources. The buoyancy of the water will help you perform movements that you might not be able to do on land where gravity is resistant to movement. Sharp movements are for resistance exercises and can be done with body parts that have movement.
Be prepared for your day in the pool by performing your bowel program prior to your swim. You might want to wear an adult protection garment. Cover any open areas with waterproof dressings to keep the pool water out of your body such as an open pressure injury site or suprapubic catheter opening. Be sure you discuss the idea of aquatic therapy with your health professional before starting to make sure it is safe for your specific and individual needs.
There are wheelchair sports groups that are available in many areas. These will help with general health but most often body parts with lack of movement are strapped down so not much activity is gained to affected limbs. However, you will breathe deeply and get a good workout to your moving body.
Activity can affect your mental health in a positive way so whatever you decide to do will be a great start. For all individuals, making time for activity is a challenge. It takes effort, thought and planning to develop an exercise plan. You can find out what others are doing or talk with your health professional who is a good conduit of sharing information.
Medication
There are medications that are being developed to help reduce the impact of injury to your body. Some of these are specific for disease processes and some for trauma. Swelling or edema is a process that occurs whenever the body is injured anywhere-even a paper cut. Swelling in the spinal cord or brain leads to complications because these body parts are contained in rigid skulls and vertebrae. Bones do not expand to accommodate swelling which puts increased pressure on tissue and nerves. Therefore, reducing the body’s natural protection of swelling at the site of injury can reduce secondary complications and injury to the central nervous system.
Typically, the medications that prevent tissue damage from traumatic spinal cord injury are used in the early hours of injury. Sometimes, the use of these medications is not recommended depending on individual situations. Researchers are looking into ideas to better understand when and how medications should be used to benefit individuals at the time of injury.
There are medications that will help with problems that come up after injury. Medications for spasticity, infection, bowel function, bladder control and many, many others, help to keep your body functioning well and can prevent further issues. Care always must be taken regarding medication, both prescriptive and over the counter as interactions do occur. Always report your full list of medications and have a professional monitor what you are taking to avoid interactions with the medication, supplements and food.
As scientist learn more about how the nerves in your body work, connect and transmit messages, more medication treatments will be developed that will assist with nerve signaling as well as to enhance function and eventually healing.
Surgery
There are surgical treatments available now that will help improve function. Surgery can be performed on peripheral nerves (those in the body) but not yet on central nerves (those in the spinal cord or brain). Peripheral nerve surgery includes nerve releases, transfers and grafting. This area of surgery is probably the most explored. Some surgeries are approved and offered in specialty centers but not yet widespread to find locally. Hand and arm nerve surgery can improve arm function. There are also some peripheral nerve surgeries that improve lower extremity function, bowel, bladder and sexual function.
Stem cell therapies and genetic manipulation procedures are being studied by researchers to promote regeneration and recovery of function after spinal cord injury. Many of these treatments may include surgery however, as more knowledge is gained, these treatments may become intravenously (IV) delivered. Stem cells and genetic engineering therapies target improved recovery of function by rebuilding damaged or lost spinal nerve circuits. While these techniques are still largely experimental, scientists ae excited about translating them to the clinic, for use either alone or in combination with other interventions (for example, certain kinds of activity-based rehabilitation).
Peripheral nerve surgery is possible and is performed by specialty trained surgeons. Peripheral nerves are outside of the brain and spinal cord. Surgery to the nerves in the peripheral nervous system (PNS) are available which includes improving function in the cauda equina section of the lower spinal cord. These nerves can be rerouted or even split to improve function. Therapy is used to help your brain and body learn to activate this reorganization.
In the Big Idea, an FDA-approved feasibility study, 36 individuals with chronic, complete spinal cord injury are being implanted with an epidural stimulator. Investigators hope to demonstrate that epidural stimulation (ES) can improve functions such as cardiovascular, sexual and bladder function, as well as the ability to facilitate standing and voluntary movements. ES raises the level of excitability in the network of nerve cells that remains intact below the level of injury; combined with appropriate sensory information, that network is able to control complicated movements.
As of July 2020, a total of 14 Big Idea research subjects had been implanted and are in varying stages of their two-year Big Idea participation. At the end, each has the option to keep the implanted stimulator or have it removed.
The Big Idea builds on a promising earlier study in which eight men were implanted with stimulators. The Christopher & Dana Reeve Foundation provided significant funding for that initial research, as well as the Big Idea. Every study of spinal cord injury repair increases the knowledge base.
More than likely, a combination of all these treatments will be used to restore function from paralysis. Activity will be needed both before and after treatment to bring the body to full recovery. Medications are used now to help people function in their daily lives but other medications specifically for recovery are being developed. Surgery to restore nerve function is underway. We have never been so close but when you are the one waiting, it can seem like forever. Now is the time to have the most hope.
Clinical Practice Guidelines
Clinical practice guidelines are available to model standards for healthcare professionals and the public about rehabiliation strategies. The Paralyzed Veterans of America have a wide variety of evidence-based guidelines available free of charge.
Spinal Network has a wide range of clinical practice guidelines.
The American College of Physicians
The American Academy of Physical Medicine and Rehabilitation provides a wide array of information at their website.
Research
Research into recovery from spinal cord injury is being conducted. There are many options that are being studied. These include therapies to preserve and restore function, medications and surgeries. The amount of information being currently being produced is mind boggling. There are even options that are available today but beware, many of the treatments being pushed on the web are not proven and can cost hundreds of thousands of dollars. Participation in some of these therapies might even keep you from benefitting from successful treatments at a later time.
There are many people ready to take you money for a ‘treatment’ that is unproven. Most of these procedures seem to be surgical although there are unproved other treatments as well. In the past, offerings for shark tissue to be placed in your back or stem cell treatments in other countries have been advertised. People have spent large amounts of money on these types of treatments. Why are they not used as often now? Because they did not produce the results promised. Sometimes, the failure was accounted to an inability to be able to measure outcomes and yet outcome measures are readily available and standardized around the world.
Waiting for recovery has always been an issue. It is easy to be drawn into false promises. As a consumer, there is a phrase, if it appears too easy, it probably is not worth it. If someone approaches you about a quick fix treatment, you should question why the rest of the world does not know about or is not using that particular therapy. A proven therapy will be known by legitimate researchers and provided to the entire SCI community.
However, there has never been a time when so much progress has been made in the treatment of spinal cord injury. These studies as well as research into specific diseases that lead to paralysis are being shared and combined to enhance your opportunities. There is no magic answer, but options do exist.
Outcomes of spinal cord injury do not rest on a medical or trauma cause. When healthcare professionals speak about spinal cord injury, they are referring to both causes. Sometimes people think little attention is paid to medical causes because research about spinal cord injury focuses on trauma. This is because trauma often provides information about the exact time of onset and level of injury. Medical causes do not have specific onset time as that is usually unknown. Medical causes of SCI usually begin prior to diagnosis. Level of injury can be variable in medical causes and often there are several injury points. Research of SCI from medical or trauma causes benefit all individuals with spinal cord injury. Research of the medical causes is usually conducted under that disease diagnosis. SCI research focuses on the injury from medical and trauma sources, curbing the injury, reducing secondary effects and cure.
Basic Science are experiments that take place in a laboratory. These experiments are important to demonstrate the possibility of treatment success in humans. They cover all aspects of SCI injury and recovery from molecular physiologic processes to drug treatment.
Clinical Research is performed with humans as the subjects. This can include physiologic, biologic, and psychologic studies. Clinical research is only done when bench science has collected enough evidence to know there is basic safety for the study to be conducted with humans.
Activity Based Therapy has been demonstrated as a key factor in spinal cord injury recovery both in active patterned movement as well as through internal and external functional electrical stimulation. In this therapy, nerves are stimulated for function from an external source or implant. When the nerve is stimulated, movement of the body occurs. The efficacy of this therapy has been demonstrated through a variety of sources.
Stem Cell Transplant for improved nerve transmission is being studied. The idea is that stem cells can be converted into any cell of the body. Creating nerve stem cells for implantation in the spinal cord is a goal but this is not yet totally effective. Currently, there is no appropriate stem cell transplant for spinal cord injury. Much progress has been made in the laboratory with animals but the translation to humans has not been made. How stem cells will become a part of spinal cord injury treatment has not yet been established.
Technology and Devices are being developed rapidly. These can include studies of implants in humans to equipment to improve function and decrease secondary complications.
An example of technology is the evolution of external electrodes for muscle movement that has evolved into microchips implanted which allow the individual to move. Further testing is underway.
Devices to assist with movement for the goal of improving ability to perform activities of daily living are being developed. These include devices for hand and arm movement to allow self-feeding, grooming and toileting assistance to mobility devices to increase range over rough or sandy terrain.
Medication for spinal cord stabilization and for secondary complications are a critical part of spinal cord injury research. Neuropathic pain leads the way as a need verbalized by individuals with spinal cord injury. Controlling spasticity is a part of controlling pain. Treatment to reduce secondary damage at the time of injury and immediately following is important to reducing the outcome of SCI. Every aspect of SCI treatment is being considered to improve quality of life.
Nerve Transfers are being studied. This can include moving a nerve from one target muscle to another, grafting a nerve to a new area, splitting a nerve so it can perform more than one function. Researchers are studying how to transplant nerves from one person to another although rejection has not yet been mastered due to the low immune system function of those with spinal cord injury. Most successful has been nerve transfers to improve arm and hand function. Transfers in the legs and to the bladder have also been successful but less functional in the legs due to balance issues. The number of surgeons who have been educated to perform this type of surgery are few.
Phrenic Stimulation is a process that increases the diaphragm to be stimulated for effective breathing. This process reduces the need for mechanical ventilation. The number of surgeons educated to perform this surgery through a minimally invasive technique is low.
Spinal Cord Injury Facts and Figures
SCI from medical and trauma causes
A 2013 survey performed by researchers at the Christopher and Dana Reeve Paralysis Foundation indicates 1.7 percent of the U.S. population, or 5,357,970 people self-identify as living with some sort of paralysis. This number includes those with a central nervous system medical diagnosis as well as trauma. Estimating the total number of individuals with spinal cord injury is challenging as those with SCI as a complication from medical illness do not necessarily identify as having a spinal cord injury but rather identify with their diagnosis.
Medical Causes of Spinal Cord Injury
There are many medical diagnoses that can result in spinal cord injury. Most individuals do not think of themselves as having a spinal cord injury but rather attribute their injury by their diagnosis. It is perfectly natural to think of disease by the medical diagnosis or cause, however, the consequences of the medical diagnosis is spinal cord injury. Other parts of the body may also be affected by the medical diagnosis especially the brain since it is part of the central nervous system. Additional complications can be attributed to spinal cord injury.
Medical causes of spinal cord injury can include the following and others:
- Amyotrophic lateral sclerosis (ALS)
- Arteriovenous malformation (AVM)
- Cerebral palsy
- Friedreich’s Ataxia
- Guillain-Barré syndrome
- Leukodystrophies
- Lyme disease
- Mitochondrial Myopathy
- Multiple sclerosis (MS)
- Muscular dystrophy (MD)
- Neurofibromatosis
- Parkinson’s Disease (PD)
- Post-polio syndrome
- Spina bifida
- Spinal muscular atrophy
- Spinal tumors
- Stroke (Brain or Spinal Cord Stroke)
- Syringomyelia and tethered cord
- Transverse myelitis
SCI from trauma
There are approximately 17,730 new cases of Spinal Cord Injury from trauma each year with an annual total of 291,000. Men number 78% of the total.
Causes of Spinal Cord Injury from Trauma since 2019
- Automobile Crashes (39.3%)
- Falls (31.8%)
- Violence (13.5%)
- Sports (8%)
- Medical Surgical Complications (4.3%)
- Other (3.1%)
- Other (16.9)
Background of individuals with spinal cord injury from trauma
- Caucasian 59.5%
- Black 22.6%
- Other 17.9%
Level of injury from trauma
- Incomplete Tetraplegia 47.6%
- Incomplete Paraplegia 19.9%
- Complete Paraplegia 19.6%
- Complete Tetraplegia 12.3%
- Normal 0.6%
Life expectancy is only slightly reduced for those with spinal cord injury with shorter life expectancy with a higher level of injury. The most common cause of death is infection, specifically pneumonia followed by septicemia.
These data are obtained from: National Spinal Cord Injury Statistical Center, Facts and Figures at a Glance. Birmingham, AL: University of Alabama at Birmingham, 2019.
A History of Spinal Cord Injury in the United States
There are many diseases that lead to spinal cord injury. In fact, that is the cause of most spinal cord injuries. People do not often think about the consequences of disease as spinal cord injury but focus on the disease itself. Because of this, some individuals tend to overlook the SCI ramifications.
With disease, spinal cord injury can progress slowly. In trauma, spinal cord injury can develop in a second. The trajectories of disease onset compared to trauma onset are typically opposite. Disease takes time. Trauma happens in an instant. With either onset, the effects of spinal cord injury or any paralysis are life altering.
Treatments have been developing for paralysis for thousands of years. Due to the pooling of information and cooperation of scientists, coordination of research findings has been crossing diagnostic boundaries. What is discovered in one neurologic disease has been translated into other neurologic diseases. Information from research of one diagnosis is often applied to other unrelated diagnoses with successful outcomes and certainly knowledge building.
Spinal cord injury has been recorded in the hieroglyphs of Egypt. You can imagine the trauma that might have been sustained by workers of the great pyramids. This would be one of the first recorded industrial accidents. Pictorial evidence of urinary catheterization has been recorded by these early historians. It seems that spinal cord injury and other paralysis have been with us since the dawn of mankind.
In some of the remains of the Native American culture in the United States, vertebrae bones with arrows going through them have been found. One arrow pierced vertebra can be seen at Cahokia Mounds in Southern Illinois. This exhibited specimen is of a human vertebra with the arrow and tip through the bone. The human tissue is long gone but the injury that would have been sustained would clearly have been a traumatic spinal cord injury.
War and trauma were the common sources of SCI for years mostly because people did not live long enough to see much effect of SCI from disease. Because of the large numbers of injured soldiers from each battle, techniques to save lives were developed over time. The more soldiers that could be saved would mean more soldiers that could return to the battlefield.
One of the first rehabilitation nurses was Florence Nightingale who suggested novel treatments such as hand washing, cleanliness in providing care and pressure release treatments. Florence thought patients should be turned to avoid pressure injury about every two hours-sound familiar? We still aim for the two hour turn in hospitals today, even though scientific evidence indicates that pressure releases should be accomplished as frequently as every 10 minutes.
Fast forward to World War II. The intervention of antibiotics and field hospitals with quick treatments resulted in a significant survival of wounded soldiers. Regenerative techniques were developed to improve vascular function and spare nerve damage. Medical doctors and surgeons continued with development of treatments after the war since many soldiers lived to return home. Today, military and other researchers continue with advancing treatments for rehabilitation care.
Paralysis treatment was extensively developed with the polio epidemic in the United States. Other countries had been conducting research for neurological conditions as well. Some of these techniques were further developed for the treatment of polio. These included providing activity to affected parts of the body, aquatic or water therapy and ventilation with iron lungs.
In polio treatment centers, those affected were provided range of motion by volunteers for hours at a time. This constant movement provided the body with the necessary activity that was not being provided internally. Aquatic therapy, in warm water, relaxed muscles and provided the buoyancy to help support limbs. Moving a body part on your own might be too difficult due to gravity but the added buoyancy of the water reduced the difficulty of overcoming gravity with movement. Another essential element for treatment was ensuring oxygenation for those who had difficulty breathing. This allowed individuals a chance to survive until enough strength was regained to participate in additional therapies. There were other treatments as well, but these were the mainstays of the program.
There were ‘spas’ that were developed around the country to provide treatments. Whole communities would take part in providing this time intensive therapeutic treatment. One famous spa is in Warm Springs, Georgia. This was developed by President Franklin D. Roosevelt for his and other’s treatment. He continued with this therapy throughout his life.
Another proponent of therapy for polio was Sister Kenny who created a novel treatment. The Sister designation was from her origin of Australia, although she did not have formal training as a nurse. Her treatment consisted of reducing spasms, so limbs could be put through range of motion. At the time, this practice was controversial as it was not the state of the art. However, her unusual thinking changed the way treatments were conducted.
In the 1990’s, much more about the workings of nervous system had been proposed. A new idea was conceived: hope. There was a wave of movement that it would be possible for individuals with spinal cord injury to improve. It was due to several discoveries such as nervous system plasticity where it is acknowledged that the nervous system can adapt to injury and reroute itself.
Previously, the nervous system was thought that only one particular nerve could connect to another particular nerve. If you think of a ponytail hair do, it was thought that if the ponytail was cut, each single hair would have to be reattached to its original hair. This was the same thinking that spinal cord injury could be repaired, each nerve reattaching to its original nerve. The concept of plasticity changed this idea. The body can adapt and adjust to injury.
There were several other major discoveries about the nervous system which when combined created a new vision of recovery from spinal cord injury. The major proponent of these discoveries was Christopher Reeve who developed what is now called the Christopher and Dana Reeve Paralysis Foundation to expand and develop these new ideas about the nervous system. His motto, Forward, indicates the need to look toward these new ideas of hope and recovery rather than to cling to old ideas that we now know did not encompass spinal cord injury recovery.
Many researchers and health care professionals have embraced the new concept of recovery for spinal cord injury. Similar therapies like those instituted for the treatment of polio have been adapted and revised for the current use. The explosion in the development of technology has been utilized to develop equipment that can replace the large numbers of people needed to deliver the therapies as well as to deliver treatments in less time allowing the recipient to have time for other pursuits in life.
As time moves on, these therapies have been refined and tested with positive results. Knowing which therapy to be provided for the best results and the length and number of treatments is being considered. Further advances in technology have allowed some of the external cumbersome equipment to be reduced to microscopic size which can actually be transplanted into the body. This is beneficial and convenient for the person with spinal cord injury.
Future research will make these technologies more encompassing and available for everyone with spinal cord injury. One of the prime features is that these technologies will benefit individuals with new spinal cord injuries and those that have injuries from years ago.
Consumer Resources
If you are looking for more information about spinal cord injury or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm ET.
Additionally, the Reeve Foundation maintains a spinal cord injury fact sheet with additional resources from trusted sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to organizations and associations which feature news, research support, and resources, national network of support groups, clinics, and specialty hospitals.
The National Institute of Neurological Disorders and Stroke
US National Library of Medicine
National Library of Medicine National Institutes of Health
The American Neurological Society
Agency for Healthcare Research and Quality
National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR)
American Association of Neurological Surgeons
FURTHER READING
Understanding the Spinal Cord section:
Bican O et al. The spinal cord: a review of functional neuroanatomy. Neurol Clin. (2013).
Montalbano MJ et al. Innervation of the blood vessels of the spinal cord: a comprehensive review. Neurosurg Rev. (2018).
Spinal Cord Injury section:
Eckert MJ et al. Trauma: Spinal Cord Injury. Surg Clin North Am. (2017).
Galeiras Vázquez R et al. Update on traumatic acute spinal cord injury. Part 1. Med Intensiva. (2017).
Mourelo Fariña M et al. Update on traumatic acute spinal cord injury. Part 2. Med Intensiva. (2017).
Other Types of SCI section:
Diaz E et al. Spinal Cord Anatomy and Clinical Syndromes. Semin Ultrasound CT MR. (2016).
Weidauer S et al. Spinal cord ischemia: aetiology, clinical syndromes and imaging features. Neuroradiology. (2015).
Greene, N.D.E., Leung, K-Y., Gay, V., Burren, K., Mills, K., Chitty, L.S., Copp, A.J. (2016). Inositol for the prevention of neurol tube defects: A pilot randomized controlled trial. Br J Nutr. 115 (6), 974-983. doi: 10.1017/S0007114515005322
Body Areas Controlled by Spinal Cord Sections section:
Bican O et al. The spinal cord: a review of functional neuroanatomy. Neurol Clin. (2013).
de Girolami U et al. Spinal cord. Handb Clin Neurol. (2017).
Ikeda K et al. The respiratory control mechanisms in the brainstem and spinal cord: integrative views of the neuroanatomy and neurophysiology. J Physiol Sci. (2017).
Diagnosing SCI section:
Zaninovich OA et al. The role of diffusion tensor imaging in the diagnosis, prognosis, and assessment of recovery and treatment of spinal cord injury: a systematic review. Neurosurg Focus. (2019).
Treatment for SCI section:
MacGillivray MK, Mortenson WB, Sadeghi M, Mills PB, Adams J, Sawatzky BJ. Implementing a self-management mobile app for spinal cord injury during inpatient rehabilitation and following community discharge: A feasibility study. J Spinal Cord Med. 2019 May 15:1-9. doi: 10.1080/10790268.2019.1614343. [Epub ahead of print]
Neal CJ, McCafferty RR, Freedman B, Helgeson MD, Rivet D, Gwinn DE, Rosner MK. Cervical and Thoracolumbar Spine Injury Evaluation, Transport, and Surgery in the Deployed Setting. Mil Med. 2018 Sep 1;183(suppl_2):83-91. doi: 10.1093/milmed/usy096.
Recovery from SCI section:
Wang Z et al. Autophagy protects against PI3K/Akt/mTOR-mediated apoptosis of spinal cord neurons after mechanical injury. Neurosci Lett. (2017)
Secondary Conditions from SCI section:
Bye EA, Harvey LA, Glinsky JV, Bolsterlee B, Herbert RD. A preliminary investigation of mechanisms by which short-term resistance training increases strength of partially paralysed muscles in people with spinal cord injury. Spinal Cord. 2019 May 15. doi: 10.1038/s41393-019-0284-2. [Epub ahead of print]
Bragge P, Guy S, Boulet M, Ghafoori E, Goodwin D, Wright B. A systematic review of the content and quality of clinical practice guidelines for management of the neurogenic bladder following spinal cord injury. Spinal Cord. 2019 Apr 10. doi: 10.1038/s41393-019-0278-0. [Epub ahead of print] Review.
Rehabilitation section:
Kornhaber R, Mclean L, Betihavas V, Cleary M.A systematic review of the content and quality of clinical practice guidelines for management of the neurogenic bladder following spinal cord injury. J Adv Nurs. 2018 Jan;74(1):23-33. doi: 10.1111/jan.13396. Epub 2017 Aug 17. Review.
Jörgensen S, Hedgren L, Sundelin A, Lexell J. Global and domain-specific life satisfaction among older adults with long-term spinal cord injury. J Spinal Cord Med. 2019 May 17:1-9. doi: 10.1080/10790268.2019.1610618. [Epub ahead of print]
Research section:
Yi Ren and Wise Young, “Managing Inflammation after Spinal Cord Injury through Manipulation of Macrophage Function,” Neural Plasticity, vol. 2013, Article ID 945034, 9 pages, 2013. https://doi.org/10.1155/2013/945034.
Lucia Machova Urdzikova, Jiri Ruzicka, Michael LaBagnara, Kristyna Karova, Sarka Kubinova, Klara Jirakova, Raj Murali, Eva Sykova, Meena Jhanwar-Uniyal, and Pavla Jendelova, “Human Mesenchymal Stem Cells Modulate Inflammatory Cytokines after Spinal Cord Injury in Rat,” International Journal of Molecular Sciences, vol. 15, no. 7, pp. 11275–11293, 2014.
Xiang Zhou, Xijing He, and Yi Ren, “Function of microglia and macrophages in secondary damage after spinal cord injury,” Neural Regeneration Research, vol. 9, no. 20, pp. 1787–1795, 2014.
Crowe, Maria J., Bresnahan, Jacqueline C., Shuman, Sheri L., Masters, Jeffery N., Beattie, Michael S., Apoptosis and delayed degeneration after spinal cord injury in rats and monkeys. Nature Medicine, vol. 3, no. 1, pp. 1546-170, 1997. https://doi.org/10.1038/nm0197-73
Activity Based Therapy section:
Behrman AL et al. Activity-Based Therapy: From Basic Science to Clinical Application for Recovery After Spinal Cord Injury. J Neurol Phys Ther. (2017).
Quel de Oliveira C et al. Effects of Activity-Based Therapy Interventions on Mobility, Independence, and Quality of Life for People with Spinal Cord Injuries: A Systematic Review and Meta-Analysis. J Neurotrauma. (2017).
Jones ML et al. Activity-based therapy for recovery of walking in individuals with chronic spinal cord injury: results from a randomized clinical trial.Arch Phys Med Rehabil. (2014)
Stem Cell Transplant section:
Khan S et al. A Systematic Review of Mesenchymal Stem Cells in Spinal Cord Injury, Intervertebral Disc Repair and Spinal Fusion. Curr Stem Cell Res Ther. (2018).
Stenudd M et al. Role of endogenous neural stem cells in spinal cord injury and repair. JAMA Neurol. (2015).
Ruzicka J et al. A Comparative Study of Three Different Types of Stem Cells for Treatment of Rat Spinal Cord Injury. Cell Transplant. (2017).
Technology and Devices section:
Angeli CA, Boakye M, Morton RA, Vogt J, Benton K, Chen Y, Ferreira CK, Harkema SJ. Recovery of Over-Ground Walking after Chronic Motor Complete Spinal Cord Injury. N Engl J Med. 2018 Sep 27;379(13):1244-1250. doi: 10.1056/NEJMoa1803588. Epub 2018 Sep 24.
Rath M, Vette AH, Ramasubramaniam S, Li K, Burdick J, Edgerton VR, Gerasimenko YP, Sayenko DG. Trunk Stability Enabled by Noninvasive Spinal Electrical Stimulation after Spinal Cord Injury. J Neurotrauma. 2018 Nov 1;35(21):2540-2553. doi: 10.1089/neu.2017.5584. Epub 2018 Jul 5.
Crawford A et al. Detecting destabilizing wheelchair conditions for maintaining seated posture.Disabil Rehabil Assist Technol. (2018).
Medication section:
Rigo FK, Bochi GV, Pereira AL, Adamante G, Ferro PR, Dal-Toé De Prá S, Milioli AM, Damiani AP, da Silveira Prestes G, Dalenogare DP, Chávez-Olórtegui C, Moraes de Andrade V, Machado-de-Ávila RA, Trevisan G. TsNTxP, a non-toxic protein from Tityus serrulatus scorpion venom, induces antinociceptive effects by suppressing glutamate release in mice. Eur J Pharmacol. 2019 May 3;855:65-74. doi: 10.1016/j.ejphar.2019.05.002. [Epub ahead of print]
Hu Y, Liu Q, Zhang M, Yan Y, Yu H, Ge L. MicroRNA-362-3p attenuates motor deficit following spinal cord injury via targeting paired box gene 2. J Integr Neurosci. 2019 Mar 30;18(1):57-64. doi: 10.31083/j.jin.2019.01.12.
Holtz KA et al. Arch Phys Med Rehabil. (2017) Prevalence and Effect of Problematic Spasticity After Traumatic Spinal Cord Injury. Spinal Cord Injury Facts and Figures
Nerve Transfers section:
Further Reading:
Hill EJR, Fox IK. Current Best Peripheral Nerve Transfers for Spinal Cord Injury. Plast Reconstr Surg. 2019 Jan;143(1):184e-198e. doi: 10.1097/PRS.0000000000005173. Review.
Peterson CL, Bednar MS, Murray WM. Effect of biceps-to-triceps transfer on rotator cuff stress during upper limb weight-bearing lift in tetraplegia: A modeling and simulation analysis. J Biomech. 2019 May 8. pii: S0021-9290(19)30319-7. doi: 10.1016/j.jbiomech.2019.04.043. [Epub ahead of print]
Phrenic Stimulation section:
Warren PM, Steiger SC, Dick TE, MacFarlane PM, Alilain WJ, Silver J. Rapid and robust restoration of breathing long after spinal cord injury. Nat Commun. 2018 Nov 27;9(1):4843. doi: 10.1038/s41467-018-06937-0.
Mantilla CB, Zhan WZ, Gransee HM, Prakash YS, Sieck GC. Phrenic motoneuron structural plasticity across models of diaphragm muscle paralysis. J Comp Neurol. 2018 Dec 15;526(18):2973-2983. doi: 10.1002/cne.24503. Epub 2018 Nov 8.

