Guillain-Barré Syndrome
The nervous system consists of two parts, the Central Nervous System (CNS) which is the brain and spinal cord and the Peripheral Nervous System (PNS) that includes all the other nerves throughout the body. Guillain Barré Syndrome (GBS) results from an attack by the body’s immune system on the peripheral nerves of the body. GBS does not affect the CNS, so thinking is not affected.
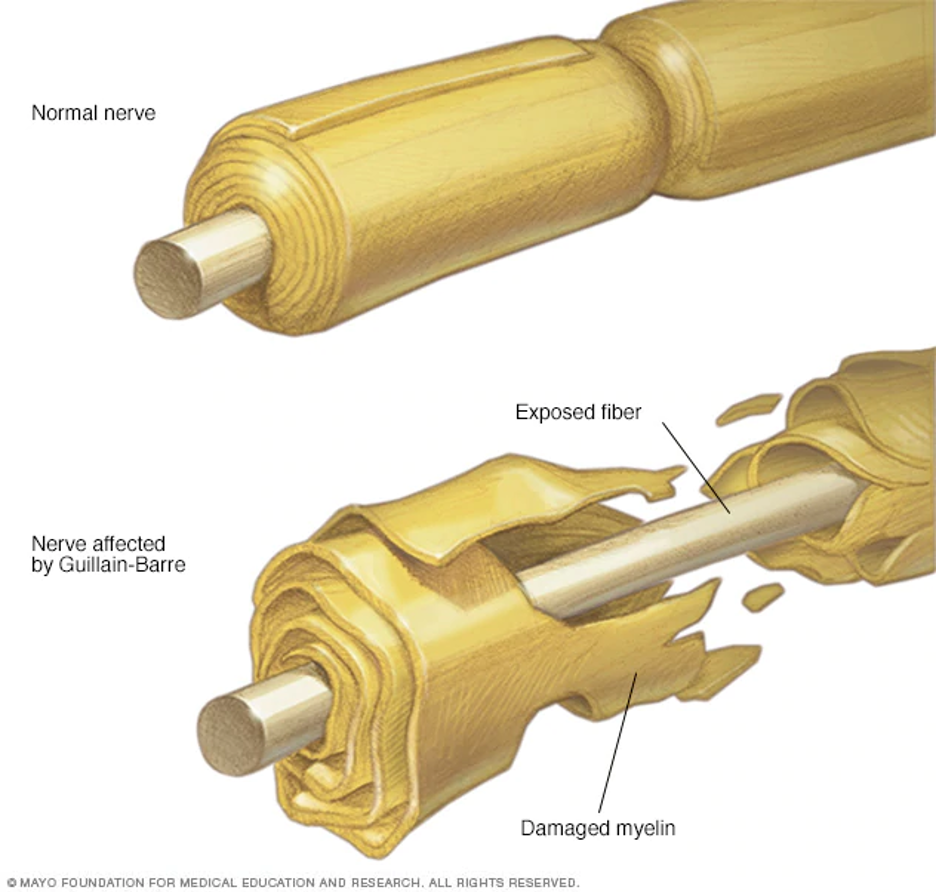
The process of Guillain Barré Syndrome is due to the immune system’s mistake in identification of normal peripheral nerve tissue as foreign. The reason for this error is unclear. The attack on the peripheral nerves causes damage to the myelin (the sticky white substance that coats the nerve.) In some cases, myelin is destroyed resulting in direct damage to the nerve fiber. One theory for the autoimmune response is the thought that peripheral nerve fibers might be attacked because they may have some characteristics that resemble bacteria or viruses.
Some believe the cause of Guillain Barré Syndrome might be due to an infection about six weeks prior to symptoms which triggers an autoimmune response (where the immune system attacks normal body tissue.) Approximately two thirds of individuals who develop GBS report a history of a respiratory, gastrointestinal or Zika virus within that six weeks window. Some specific viruses have been connected with GBS including Campylobacter jejuni, cytomegalovirus (CMV), Mycoplasma pneumonia, Epstein–Barr virus, and influenza virus. Other, rare triggers for GBS include surgery or other illnesses. The exact cause of Guillain Barré Syndrome is unknown.
Guillain Barré Syndrome occurs in two phases. The acute phase occurs when the symptoms are developing. Then there is a plateau. The recovery phase begins when symptoms start resolving. In the acute phase, symptoms ascend (goes up) the body. During recovery, resolution of symptoms descends (goes down) the body sometimes completely and sometimes partially.
In about ten percent of cases, reverse GBS occurs. In reverse GBS the symptoms travel down the body, starting at the face, with weakness descending (moving down) the body instead of going up. Recovery of reverse GBS occurs with resolution of symptoms going up the body.
Guillain Barré Syndrome affects both the motor nerves and sensory nerves of the body. The first symptoms of GBS begin as weakness, pain, numbness and tingling most often in the feet and hands. Symptoms are equal on both sides of the body. Weakness is typically noted in the legs with decreased ability to walk or to climb stairs. Pain is sometimes seen in adults. Pain is more pronounced in children and it may cause them to refuse to walk.
As Guillain Barré Syndrome advances, the muscles of the body become weak eventually developing flaccid paralysis. Due to the disruption of myelin coating, messages cannot be effectively transmitted. If the respiratory muscles are affected, assistance by mechanical ventilation may be needed to maintain breathing. The autonomic nervous system (ANS), the functions of the body that are automatically controlled by the nervous system, can be affected producing cardiac problems such as a slow or irregular heartbeat and changes in blood pressure.
The onset of GBS progression is within hours or days. Symptom progression is very individualized. Some will have a quicker progression and some longer. The range of progression of Guillain Barré Syndrome can occur over a matter of hours to four to six weeks before stabilization. Symptoms peak in about two weeks for most individuals. By three weeks, 90% of affected individuals reach symptom peak. For a few individuals plateau can take up to four weeks.
The recovery process is also variable. It is possible for recovery to be swift but far more likely, resolution can take six to twelve months. For some, the resolutions process can take up to three years. Recovery can be complete or partial.
Some individuals have a complete recovery from GBS. For others, there might be some deficits that remain which will require adaptive equipment to improve function. New techniques for carrying out daily activities may be needed.
There is also a possibility that there might be some deficits that other muscle groups may be able to accommodate for these changes. However, as aging occurs, this accommodation of deficits might not be able to maintain usual function. Occasionally, a small number of individuals will have a decline in general ability which allows this remaining deficit to become more prominent.
A very small number of individuals who have GBS have a relapse of symptoms. This can be as severe as or less severe than the first incidence.
Guillain Barré was named for the French neurologists who first described it in 1916. These physicians were Georges Guillain, Jean Alexandre Barré, and André Strohl. Some refer to the syndrome as Guillain Barré Strohl. Other names for Guillain Barré Syndrome are Landry’s paralysis and postinfectious polyneuritis.
Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved.
Types of Guillain Barré Syndrome
There are specific types and subsections of GBS. Treatment options may depend on the type of GBS that occurs.
Acute Inflammatory Demyelinating Polyneuropathy (AIDP): The myelin coating of the nerve is damaged resulting in poor transmission of nerve signals.
Acute Motor Axonal Neuropathy (AMAN): The myelin coating and motor nerve fibers (axons) are damaged resulting in poor to absent transmission of nerve signals for movement and reflexes but sensory function remains.
Acute Motor-Sensory Axonal Neuropathy (AMSAN): The myelin coating, motor and sensory nerve fibers (axons) are damaged resulting in poor to absent transmission of nerve signals for movement and sensation.
Miller-Fisher Syndrome: This rare variation of Guillain-Barré syndrome has the symptoms of abnormal muscle coordination with poor balance and clumsy walking due to muscle weakness, weakness or paralysis of eye muscles, absence of tendon reflexes and respiratory failure. A unique antibody is present. It also may follow a viral illness.
Acute Pandysautonomic Neuropathy (APN): APN affects the autonomic nervous system and includes encephalopathy (damage or disease of the brain) but does not include movement or sensation. Symptoms include orthostatic hypotension (low blood pressure), inability to sweat, unreactive pupils, decreased tears and saliva production, gastrointestinal dysfunction, and impaired urinary and sexual function.
Related peripheral nerve disorders:
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP): CIDP consists of progressive weakness in large numbers of nerve groups over many years. It is thought to be a chronic form of GBS.
Multifocal Motor Neuropathy (MMN): MMN affects multiple muscles in a part of an arm or leg (smaller numbers of nerve groups), typically on one side of the body.
Symptoms of Guillain Barré Syndrome
Guillain Barré is a syndrome because it consists of a group of symptoms that generally occur together. Symptoms may be all or some of the following:
- Prickling, pins and needles sensations in your toes and ankles or fingers and wrists
- Severe pain that may feel achy, shooting or cramp-like and may be worse at night
- Muscle weakness in your legs that spreads to your upper body
- Incoordination and unsteadiness particularly in climbing stairs or walking
- Difficulty with bladder control, digestion and bowel function
- Difficulty with facial movements, including speaking, chewing or swallowing
- Difficulty breathing
- Difficulty moving or inability to move eyes, vision issues such as double vision
- Abnormal or rapid heart rate
- Low or high blood pressure
Diagnosing Guillain Barré Syndrome
The symptoms of GBS can be similar to several other neurological issues. The hallmark signs of GBS are symptoms appearing simultaneously on both sides of the body and with quick onset. GBS typically appears within hours as opposed to other neurological issues where symptoms evolve over months.
Physical Examination. It will be important to tell all your symptoms to your healthcare provider or emergency room providers in a physical examination to assist in diagnosis. This includes weakness and sensation changes such as numbness, tingling and pain. You will need to mention when these symptoms began, if they started in the feet and legs, hands and arms or both. Onset within hours to four weeks with equal symptoms on both sides are signs of GBS.
In the physical examination, the healthcare provider will conduct a neurological examination which will include an assessment of deep tendon reflexes using a reflex hammer on the back of the ankles, knees, wrists, elbow and other locations. Absent or diminished deep tendon reflexes are a sign of GBS.
In your health history, be sure to mention if you have had a viral illness especially within the last six weeks, diarrhea, surgery or other unusual medical issues.
Lumbar puncture or spinal tap with spinal fluid analysis. In this sterile procedure, you will be asked to lay on your side with your knees to your chest or if you are able, to sit with your knees to your chest. This opens the spaces between your vertebrae in your back. A needle will be inserted into the space that surrounds the spinal cord between L3 and L4 (the third and fourth lumbar vertebrae). A very small amount of spinal fluid will be removed and tested in the laboratory. A sign of GBS is elevated cerebrospinal fluid protein without elevated cell count.
Nerve Conduction Studies (NCS) are done by application of a small amount of electrical current to an area of a nerve to assess how well a message is conveyed by that nerve. A slow or abnormal conduction signal indicates GBS. An electromyogram (EMG) which measures how well a muscle works may also be done.
Treatment for Guillain Barré Syndrome
There is no curative treatment for GBS, but two therapies might be done to help lessen the symptoms and shorten the course of the syndrome.
Plasma exchange (plasmapheresis). In this therapy, typically your own blood is used. Blood (plasma) is separated from your blood cells. Your own blood cells are returned into your body, but your body makes more plasma to replace what was removed. Newly developed plasma should not attack the peripheral nerves.
Immunoglobulin therapy. Blood from donors is given to you. The blood contains immunoglobulin (including healthy antibodies) that can block the damaging antibodies that your own body is making. This stops the attack of the peripheral nerves leading to GBS.
Other comfort measures will be provided such as medication to control pain and to stabilize normal body functions.
If your condition requires assistance with breathing, mechanical ventilation will be provided. The type of ventilation will be selected to fit your specific requirements.
Recovery From Guillain Barré Syndrome
Recovery from GBS is variable. The general rule for recovery is the same for peripheral nerve injury, which is what occurs in GBS. Peripheral nerves recover one inch per month. Recovery of GBS depends on the amount of damage to the myelin and if it includes damage to the peripheral nerves. Just as GBS ascends the body during the acute phase, it will descend in the same manner during recovery. Some individuals will have recovery within three weeks. Many will have recovery over six to twelve months. Still others may take three years to recover.
Although most individuals recover from GBS, 4-7% of cases are fatal. Most individuals survive GBS and 60-80% are walking at six months.
Not everyone has a complete recovery. Residual issues can linger in an estimated 7-15% to 40% of individuals recovering from GBS. Typical residual issues of GBS include ongoing weakness, lack of reflexes, loss of balance or sensory loss. Neurological problems of foot drop in both feet, muscle wasting in the hands, loss of coordination due to decreased sensory input (sensory ataxia), and painful, burning, tingling or restrictive sensations (dysesthesia) may remain.
Rehabilitation For Guillain Barré Syndrome
During the acute phase of GBS, your healthcare needs will probably be provided in the intensive care unit. Strategies to maintain function and protect your body will be in place. This includes proper positioning and turning, pressure dispersing surfaces, and range of motion exercises. If you have difficulty swallowing or eating, nutrition will be supplied through an I.V. or tube feedings. Your mental health will be cared for through support, reassurance and distraction therapies.
In the recovery phase, more intensive therapies will be provided to improve function and mobility. Energy conservation and dealing with fatigue will be a concern of everyone on your recovery team as you return to function.
A Physiatrist, a medical doctor who specializes in physical medicine and rehabilitation, will direct the care and needs of your recovery.
Physical Therapists will provide therapy and guidance in movement and strengthening to learn to turn yourself, balance, sit, and walk as your recovery progresses. They will provide equipment and adaptions that will improve and enhance your recovery.
Occupational Therapists provide therapy for activities of daily living (ADLs). They help with fine motor control, bathing and dressing strategies, feeding adaptions, everything you need to help with your daily life.
Speech/Language Pathologists will assist with language skills and improvement in swallowing ability.
Registered nurses will monitor your health status, provide medications as necessary and include rehabilitation strategies into your daily routine. They will also help restore bowel and bladder control. Nurses will assist with planning your discharge to home or to temporary long-term care, if needed.
A Psychologist will help with adaption to life with this diagnosis. They will work with you to ensure your mental health is well.
A Social Worker can help with transition to home, ensuring you have the supplies you need and that your home has the needed equipment for a safe return.
Guillain Barré Syndrome and Vaccinations
Previously, there has been some discussion about the development of GBS after a flu vaccination. This thought was due to the swine flu vaccine given in 1976 because it was developed using a type of tissue which is no longer used. The swine flu vaccine was developed using brain tissue but now it is developed in eggs. The CDC (Centers for Disease Control and Prevention) has researched this issue and has found that the rate of GBS is none to 1 to 2 cases per million of flu vaccines given, similar to the general population. The risk of having the flu and then developing GBS is 17.2 per million. Therefore, the chance of contracting GBS is greater if you get the flu than if you get the flu vaccine.
Studies indicate no additional risk in developing GBS with any of these vaccinations: measles, mumps, rubella, HPV, meningococcal conjugate, polio, pneumococcal, varicella, Hib, rabies, tetanus, diphtheria, hepatitis A, and hepatitis B. https://www.chop.edu/centers-programs/vaccine-education-center/vaccines-and-other-conditions/guillain-barre-syndrome
Discuss with your healthcare provider if you should get the flu vaccine if you have had GBS in the past.
Research
Many aspects of Guillain Barré Syndrome are being studied. One area is the immune aspect as a trigger for the syndrome. Researchers are examining infection theory as a trigger, why the immune system targets peripheral nerves and how to stop this from happening. Once an understanding of why this happens, alternatives to stop GBS can be developed. Specifically, in GBS, anti-ganglioside antibodies are elevated in the blood. How these affect the development of GBS and how they can be controlled is under investigation.
Alternatively, there is a theory that some genetic variations may make a person more susceptible to developing GBS. This theory needs more support to identify the genetic variations and why this could be the trigger.
Facts and Figures
GBS affects approximately one person in 100,000 every year.
Acute Inflammatory Demyelinating Polyneuropathy (AIDP) is the most common form of GBS in the U.S.
Men and women are equally affected.
GBS is more frequent in adults and older people but anyone of any age can be affected.
Children, who rarely develop Guillain-Barre Syndrome, generally recover more completely and quickly than adults.
Recovery of walking independently is about 80% six months after diagnosis.
Recovery of motor strength is about 60% one year after diagnosis.
Delayed or incomplete recovery occurs in about 5% to 10% of individuals.
Relapse of GBS occurs in 2% to 5% of individuals.
Consumer Resources
If you are looking for more information about Guillain Barré Syndrome or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm ET.
Additionally, the Reeve Foundation maintains fact sheets with additional resources from trusted Reeve Foundation sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis. We encourage you to reach out to GBS support groups and organizations, including:
GBS-CIDP support group https://www.gbs-cidp.org/support/
National Institute of Neurological Disorders and Stroke https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-sheets/Guillain-Barr%C3%A9-Syndrome-Fact-Sheet
National Organization for Rare Diseases https://rarediseases.org/organizations/guillain-barre-syndrome-support-group/
A Clinical Practice Guideline for the treatment of GBS is available:
Hughes RAC, Wijdicks EFM, Barohn R, Benson E, Cornblath DR, Hahn AF, Meythaler JM, Miller RG, Sladky JT, Stevens JC. Practice parameter: Immunotherapy for Guillain–Barré syndrome, Report of the Quality Standards Subcommittee of the American Academy of Neurology, Neurology 2003;61;736-740. www.neurology.org
FURTHER READING
References
Green DM, Ropper AH. Mild Guillain-Barré Syndrome. Arch Neurol. 2001;58(7):1098-1101. doi:10.1001/archneur.58.7.1098.
Haber P, Sejvar J, Mikaeloff Y, DeStefano F. Vaccines and Guillain-Barré syndrome. Drug Saf. 2009;32(4):309-23. doi: 10.2165/00002018-200932040-00005.PMID: 19388722 DOI: 10.2165/00002018-200932040-00005.
Hiraga A, Mori M. Recovery patterns and long term prognosis for axonal Guillain-Barré syndrome. Journal of Neurology Neurosurgery & Psychiatry, 2005, 76(5):719-22 DOI: 10.1136/jnnp.2004.051136.
Hiraga A, Mori M, Ogawara K, Kojima S, Kanesaka T, Misawa S, Hattori T, Kuwabara S. Recovery patterns and long term prognosis for axonal Guillain-Barré syndrome. J Neurol Neurosurg Psychiatry. 2005 May;76(5):719-22. doi: 10.1136/jnnp.2004.051136.PMID: 15834034 PMCID: PMC1739613 DOI: 10.1136/jnnp.2004.051136. March 01, 1997; 48 (3) ARTICLE
Ho TW, Li CY, Cornblath DR, Gao CY, Asbury AK, Griffin JW, McKhann GM. Patterns of recovery in the Guillain-Barre syndromes. Neurology, First published March 1, 1997, DOI: https://doi.org/10.1212/WNL.48.3.695
Hughes RAC, Cornblath DR. Guillain-Barré syndrome. Thelancet.com, Volume 366, November 5, 2005, 1653-1666. doi:10.1016/S0140-6736(05)67665-9.
Kusunokia S, Kaidab K, Uedaa M. Antibodies against gangliosides and ganglioside complexes in Guillain–Barré syndrome: New aspects of research. Biochimica et Biophysica Acta (BBA), Volume 1780, Issue 3, March 2008, Pages 441-444. https://doi.org/10.1016/j.bbagen.2007.10.001.
Tam CC, O’Brien SJ, Petersen I, Islam A, Hayward A, Rodrigues LC. Guillain-Barré Syndrome and Preceding Infection with Campylobacter, Influenza and Epstein-Barr Virus in the General Practice Research Database. Plos One, April 4, 2007 https://doi.org/10.1371/journal.pone.0000344.

