Brain Injury
A brain injury (BI) is an event that causes a disruption in functioning. BI specifically indicates harm to the brain. When a BI is caused from a medical issue such as a stroke, tumor, metabolic issue or other medical diagnosis, the term, acquired brain injury (ABI) is used. A brain injury caused by an accident or intended harm is called a traumatic brain injury (TBI). A head injury can be any bump, cut or bruise to any part of the head but not extending into the brain. BI affects the brain.
The central nervous system (CNS) consists of the brain and spinal cord. Since the brain and spinal cord work together and are similar in tissue consistency, these two organs need to be discussed together. The brain and spinal cord are extremely delicate. Therefore, the body is built to provide them with the utmost protection, complete bone encasement. Notice these are the only two body organs that are completely housed in bone. That is a clue to their importance and need for protection.
The brain is encased in the ridged bone of the skull. The skull has room for the brain, blood flow and the cerebral spinal fluid that cushions it. There is absolutely no room for anything else. When an injury occurs to the brain, there can be an increased amount of blood, fluid, inflammation or even air which cannot be accommodated. Therefore, something less rigid than the skull will need to shift due to the extra load. The sensitive brain tissue will collapse as the extra fluid presses against it, leading to more damage. Another issue is that the swollen brain tissue can drop through the largest opening in the skull at the brainstem thereby damaging it. This is called brain herniation.
Similarly, the spinal cord is housed in the bony vertebrae or spinal bones. These bones are articulated to accommodate body movement. The same principle applies in that there is only room for the spinal cord, blood flow and cerebral spinal fluid. Injury in the spinal cord results in collapse or damage to the spinal cord tissue as the vertebral bones are also rigid.
In brain injury, there is typically an event in the brain which can be from disease or trauma. As brain cells are affected, molecules are released into nearby tissues. This creates a series of changes in the brain at a cellular or even molecular level that leads to cell death, axonal (nerve) damage and inflammation. These molecular and chemical changes lead to the chronic symptoms and deficits of brain injury.
Causes of brain injury include medical and trauma sources. The effects of brain injury can include loss of consciousness, breathing problems, alterations in thinking, and issues with body movement. Each situation of brain injury is unique depending on the location of the injury in the brain. The course of brain injury also varies from a short interruption in function to long lasting issues.
Types of Brain Injury
Spinal cord injury and a co-occurring brain injury often appear as dual diagnoses.
Since the spinal cord is connected directly to the brain, an injury to one will affect the other. The brain can be affected by an injury to the spinal cord or the spinal cord can be affected by an injury to the brain. In many cases, a brain injury is a result of damage to the spinal cord or a medical condition that affects the entire central nervous system (CNS), both spine and brain.
The amount of force required to result in a traumatic spinal cord is the same amount of force applied to the entire body including the brain. The head is a large body part supported by the smaller sized neck so a trauma to the spinal cord can reverberate as the neck is not strong enough to support the head under such dramatic circumstances. SCI from a bullet wound can produce a shock wave through the spinal cord and up inside the brain.
If there is a medical source of spinal cord injury, the same medical condition is working throughout the central nervous system tissue, including the brain. Diseases of the spinal cord and brain generally affect both due to the displacement of tissue or effects on the central nervous system nerves.
However, a spinal cord injury that occurs, from trauma or medical causes, can result in stretching, constriction, displacement, lack of oxygen, or damage to nerves of both spinal cord and brain tissue. Because of the attachment of the brain and spinal cord, an injury to one can directly or indirectly affect the other. There is far more occurrence of a spinal cord injury affecting brain function than has been previously diagnosed.
Brain injury as a result of SCI may go undiagnosed because of loss of consciousness, lack of ability to move the body or subtleness of the injury. Symptoms of brain injury may be overlooked because of the SCI experience, severe illness, anesthesia, depression, anxiety, fear, and paralysis. Many times, change in brain function is noted by family members either in the rehabilitation setting or when the individual is discharged to home where they have difficulty in performing thinking activities that they used to do with ease. Behavioral issues can appear outside of the controlled environment of a hospital.
A complication of dual diagnosis of brain and spinal cord injury is heterotrophic ossification (HO) which is abnormal bone growth into soft tissues and muscles. This can lead to joint immobility and pain. This condition can be found in individuals with BI or SCI, but the dual diagnosis of brain injury and spinal cord injury makes it more likely to develop. It can be treated with medication such as indomethacin if caught early. Later diagnosis requires surgical correction. Low dose radiation is sometimes used as a prophylaxis for HO.
Congenital Brain Injury
Brain injury can be caused from a variety of factors. If damage occurs to the brain before, during or just after birth, congenital brain damage is diagnosed. Causes of congenital brain damage include genetic issues, infections, trauma, metabolic issues in the fetus or mother, or other medical issues. Sometimes the cause is unknown. Congenital brain damage can be progressive or nonprogressive as in the example of cerebral palsy. Congenital brain damage is not typically classified as a brain injury, but the treatments may be used interchangeably.
Acquired Brain Injury (ABI)
Injury to the brain after six months of age is considered an acquired brain injury (ABI). There are various causes for ABI which are due to medical issues. Examples include:
Diseases such as multiple sclerosis (MS), Parkinson’s disease (PD), Alzheimer’s disease and other dementias, results of cancer (tumor)
Stroke from bleeding into the brain or lack of oxygenation to the brain from a blocked artery or arteries
Anoxia or lack of oxygen to the brain as in extreme hypothermia, near drowning, or suffocation
Alcohol or drug use which can poison the brain
Traumatic Brain Injury (TBI)
Traumatic Brain Injury (TBI) is the result of trauma to the brain. This can be caused by a bump, blow, or jolt that is severe enough to damage the brain. A penetrating head injury where something breaks the skull is considered a TBI. As the central nervous system (CNS) includes both the brain and spinal cord, these same trauma sources can also be found in traumatic spinal cord injury.
Mild Traumatic Brain Injury (mTBI)/Concussion
A classification of mTBI is a traumatic brain injury but the symptoms are more subtle as in a concussion. Most often symptoms are more general such as forgetfulness, neck pain, headache, and dizziness but can include symptoms such as loss of consciousness (LOC), difficulty with thinking, concentration or balance, nausea, blurred vision, sleep disturbances, and mood changes. The symptoms can be reflective of the specific part of the brain that is injured or the brain in general.
Post-Concussion Syndrome
Symptoms of concussions resolve in approximately two weeks. When symptoms continue for a month or two, post-concussion syndrome is diagnosed. The symptoms can continue when at rest, with activity or cognitive (thinking challenges). The individual may withdraw from their usual social, professional, scholastic, or physical activities.
Classifications of Injuries to the Brain
What occurs in the brain is determined by the source of the injury or resulting effects in the brain. These situations arise from medical or trauma causes. Closed head injuries occur when the skull is not penetrated. Typically, a closed head injury occurs with a significant bump, shaking or shock wave to the head. Medical issues such as stroke, tumor or any cause of loss of oxygen to the brain can result in a closed head injury. Open head injuries occur when the outer layer of the membrane that holds the brain is disrupted. Typically, the skull is broken. This can result from something penetrating the brain including a foreign object such as a knife, bullet, or tree limb or from a part of the skull that breaks away and lands in the brain.
Brain Herniation occurs when pressure or swelling inside the brain forces the brain tissue to be pushed to an area where the skull does not resist. The only spot for this to happen is an opening at the back base of the skull, about the size of a quarter, where the brain stem connects to the spinal cord. If the skull is fractured (broken), the brain can expand through the broken area. The brain tissue is squeezed or damaged as it is pushed through the protection of the skull.
Concussion is the most common type of TBI. Concussion happens when you get bumped on the head strongly enough to cause the brain to hit up against the skull. It can be mild with a brief change in mental status or consciousness, lasting from minutes to days. A severe TBI consists of an extended period of unconsciousness or memory loss. Post-concussion syndrome is diagnosed if symptoms last more than a month. There are specific treatment plans for both concussion and post-concussion syndrome.
Contusions may appear with concussions. This is a small amount of bleeding in the brain at the site of the concussion or where the brain hit the skull. The bleeding might resolve on its own as the body naturally attempts to heal itself. The extra blood is absorbed from the injured area over time. If the contusion is large, continues to bleed or is compressing brain tissue, the blood will be removed surgically.
Hemorrhage is uncontrolled bleeding on the surface of the brain (subarachnoid hemorrhage) or inside the brain (intracerebral hemorrhage). A hemorrhage in the brain or spinal cord can develop from trauma or medical issues. Hemorrhage is active bleeding.
Intracranial hematomas are collections of blood around or within the brain. Blood between the skull and brain is called an epidural hematoma, meaning outside the dura or the tough membrane that surrounds the brain. Blood below the protective dura surrounding the brain are subdural hematomas. Blood within the brain is called intracerebral hematoma (intra meaning within, cerebral meaning brain and hematoma meaning collection of blood.)
Coup-Contrecoup Brain Injury are French words for blow and counter blow. In this type of injury, a force drives the head one direction which causes the brain to hit the inside of the skull. However, the force of this type of injury is so great that after the head hits in one direction, the force then causes the brain to bounce back and hit the skull in the opposite direction. The two areas of the brain can be at the front and back, side to side, or any other angle. The result is two areas of the brain are affected.
Diffuse Axonal Injury (DAI) occurs when the nerves or axons of the brain are torn from their locations. This is from the brain being shaken or twisted inside the skull. The shaking or twisting of the brain can be from trauma or intentionally produced by shaking someone violently. Sometimes called axonal shearing, the size of the tears and number of axons injured determine the severity of the condition. These injuries can be difficult to detect as they might be so small that they cannot be seen on MRI, however even microscopic tears produce significant damage. This type of TBI is the most serious. DAI is mostly known as shaken baby syndrome, but it can occur at any age. The elderly are lesser known victims of shaking.
Penetrating Brain Injuries occur when a projectile opens the skin and skull. Typically, these projectiles might be a bullet, a knife, a tree limb, a tool, or any other implement that opens the skull and enters the brain. The projectile may pass through from one side of the skull to the other or may lodge in the brain. Any projectile should not be removed until a medical professional assesses the situation. Removal can cause increased bleeding, damage, or death.
Blast Induced (bTBI) is a result of a shock wave to the brain or through blood vessels or cerebral spinal fluid from an explosion. This type of injury is most often found in military settings but can occur in industrial accidents and other explosion type of injuries. Meth lab explosions can result in a form of blast injury. bTBI can range from mild to severe. Typically, there are other injuries associated with it such as spinal cord injury, burns, multi-trauma and post-traumatic stress disorder (PTSD).
Second impact syndrome occurs when two brain injuries happen. They can be close in timing or one injury may occur after time has passed from the first injury. This double injury can lead to an extension of the first injury or compound it with new symptoms. Individuals with a brain injury should always seek a medical evaluation if they encounter a second brain injury.
Preventing Brain Injury and Spinal Cord Injury
Those guarding against a brain injury, a second brain injury, or a spinal cord injury should follow these guidelines:
- Keep to the task at hand, avoid distractions
- Adults should wear seat belts and children should ride in safety seats in the back of the car
- Never drive while under the influence of alcohol or drugs including street and prescription medications that can impair your ability to drive.
- Wear a helmet when engaged with open vehicles, sports, anything with wheels, horse riding, skiing or snowboarding. Know the safety recommendations for these sports.
- Avoid falls in the home by using a step stool and grab bars, stairway handrails on both sides, remove throw rugs, secure electrical cords, use nonslip mats, use grab bars in wet areas, clear clutter.
- Do not dive into shallow water, push someone into a pool or water, keep the area around water clear of clutter
- Exercise to maintain health, strength, and balance, have your vision checked.
- Keep all areas well lighted.
- Keep firearms locked and secured. Keep bullets in another locked and secured area.
- To protect children, properly install and use car seats, install window guards to prevent falling out of open windows, safety gates especially at stairs, child height handrails, play at playgrounds with shock absorbing ground cover, wear safety helmets, remove clutter, stay off fire escapes and balconies.
Brain Areas of Function
There are two main parts of the central nervous system, the brain and the spinal cord. The brain is where information is processed and acted upon. The spinal cord is the transmitter of messages to and from the brain and body. Both are needed to keep the body functioning. They are interdependent. Areas of the brain control and direct specific functions. The spinal cord carries those messages to and from the body in response.
The brain consists of two sections called hemispheres with a single unit, the cerebellum, at the back base. There is a crossing of sides of hemispheres of the brain to control of the body. The right-brain hemisphere of the brain controls the left side of the body. The left-brain hemisphere controls the right side of the body.
Each brain hemisphere is divided into sections that have responsibility for certain activities. The location of the injury in the brain determines which corresponding parts of the body will have disrupted function. Injuries can affect more than one section of the brain and may extend to just one side of the brain, may involve several parts of the brain, or may affect a part of the brain with pressure injury on the opposite side.
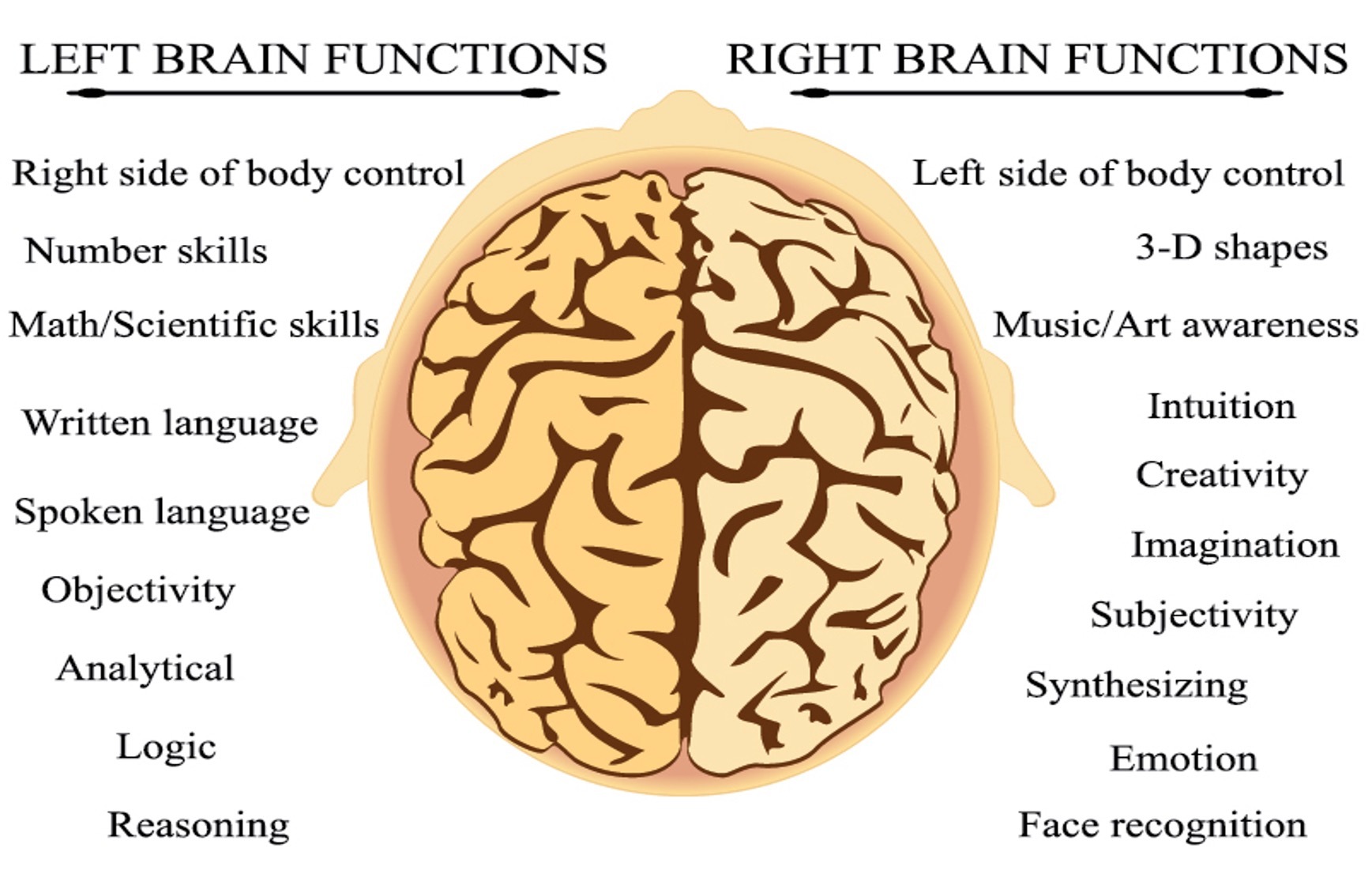
All parts of the brain work in unison. Control areas of the brain overlap in function or may rely on multiple parts of the brain to complete one activity. Sections of the brain are identified with specific processing responsibilities.
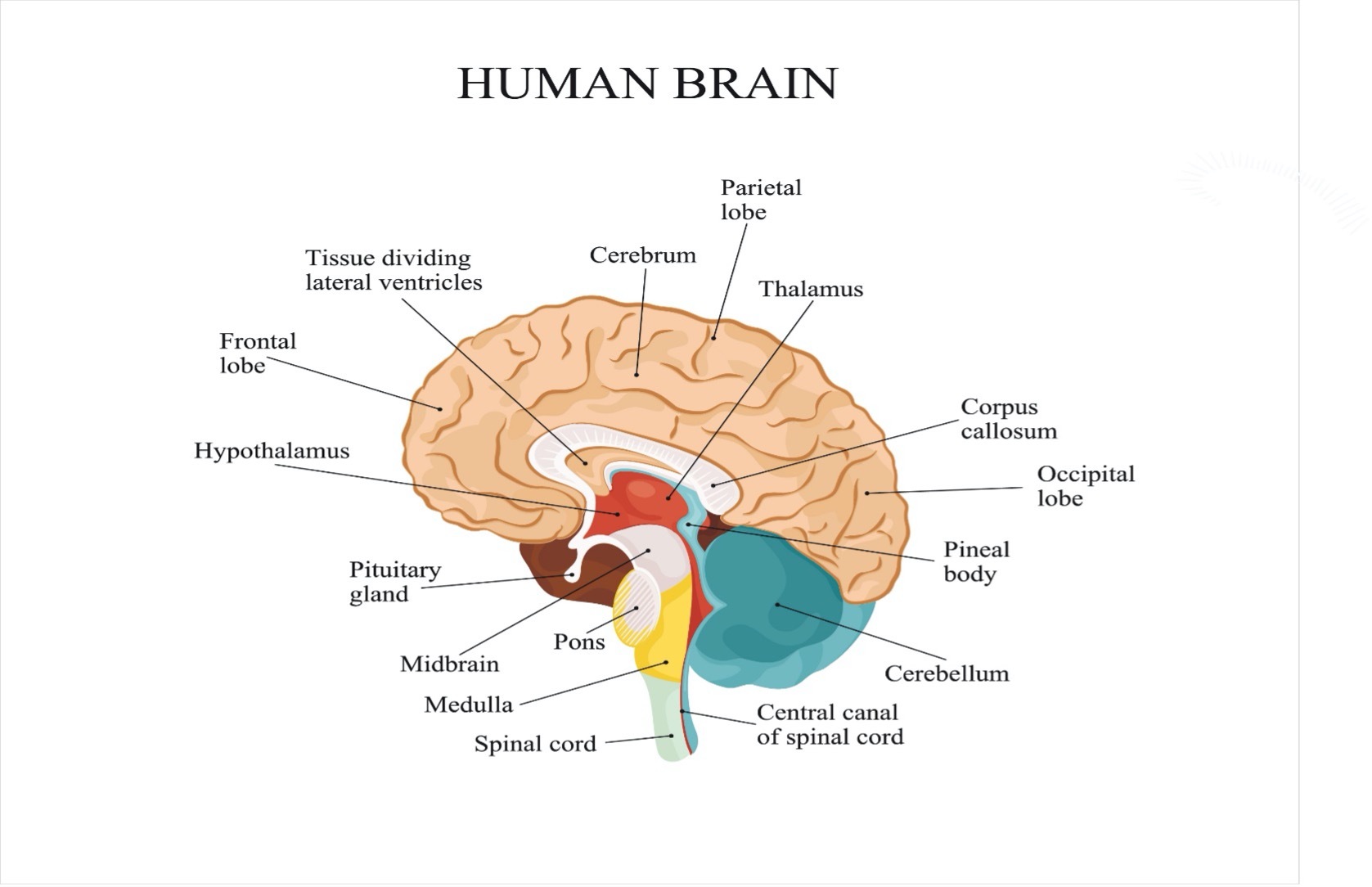
The frontal lobes are under the skull of the forehead starting a bit below the hairline to about the line of the ear. The general function of this part of the brain is for problem solving, judgement and motor function.
The parietal lobes are located at the crown of the head. This area manages sensation, handwriting, and body position.
The temporal lobes are on each side of the brain above the ear. This area is generally responsible for memory and hearing.
The occipital lobes are at the higher back of the head and are responsible for the brain’s processing of information for vision.
The cerebellum is a single unit at the back of the head just above the bottom of the skull. The cerebellum coordinates voluntary movement.
The brainstem is at the back base of the brain and connects with the spinal cord. It controls breathing and heartbeat.
Note in the drawing below the location of the sensory and motor areas which cross from side to side in the center of the brain.
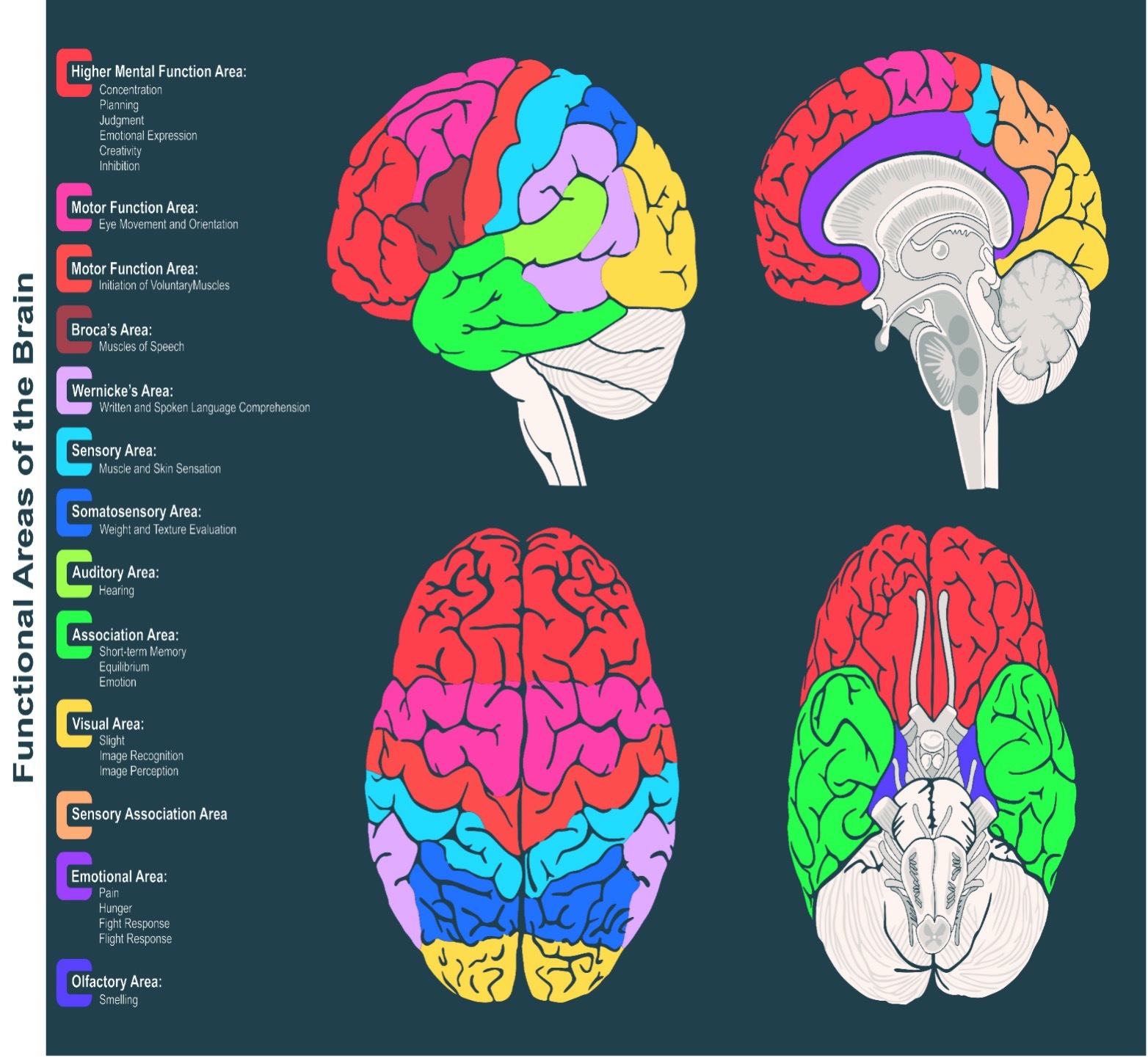
 This next image provides a more detailed map of the brain and where functions occur. Brain injuries can affect physical, cognitive (thinking) and emotional activity. Combinations of issues typically occur in brain injury.
This next image provides a more detailed map of the brain and where functions occur. Brain injuries can affect physical, cognitive (thinking) and emotional activity. Combinations of issues typically occur in brain injury.
The brain stem is the connection between the brain and the spinal cord. The brain and spinal cord work together as one unit. The brain is in control of all functions of the body while the spinal cord transmits messages to and from the body and brain. Some people try to separate the sections or sections of the brain and of the brain and spinal cord, but all body activity is dependent on the interconnection of the parts.
Issues of Levels of Consciousness in Brain Injury
Being awake, alert, and aware of our surroundings is the way most individuals perceive and interact with the world. After a brain injury, there can be various states of consciousness that affect an individual’s mentation or mental status. A person may not noticeably follow one level of consciousness to another. In fact, many individuals will be at one state and could possibly be completely awake at the next minute.
Loss of Consciousness is a temporary period where lack of awareness is due to lack of oxygen to the brain or abnormal electrical activity within the brain. Passing out, fainting, or seizures are the most common reasons for loss of consciousness. Some healthcare issues can lead to loss of consciousness such as excessive bleeding in the body. Trauma can also lead to loss of consciousness.
Coma is a state of prolonged unconsciousness. An individual is unaware of their body functions and surroundings. Medical attention is needed to preserve brain and body functions. Comas last from hours, days to weeks, rarely longer. People who are in a coma for a long period of time may move to a vegetative state where consciousness is not achieved but they may breathe on their own, move their limbs and even open their eyes. These activities may be in response to stimuli but without consistency. Persistent vegetative state is determined if the individual has been in a vegetative state for one year from onset of a brain injury, six months from lack of oxygen to the brain. Brain death occurs when all brain and brain stem function ceases. Several independent medical assessments are made and need to be in agreement to determine brain death.
Minimally conscious state occurs when the individual has some awareness. This can be a response to sound, pain, or other stimuli.
Locked-In Syndrome is a type of brain injury that affects the lower brain and brainstem but not the upper parts of the brain. This prevents any body movement, including talking, but the individual is aware of everything that is happening. There may be movement of the eyes which can be used for communication. Because of lack of responses, it can be mistaken for loss of consciousness, coma or vegetative state. The cause of locked-in syndrome can be from disease, trauma, or poisoning.
Dual Diagnosis of Brain Injury and Spinal Cord Injury One injury to the nervous system is an issue but two injuries to the nervous system in different areas compound a person’s ability to respond. A brain injury and spinal cord injury create additive symptoms as one will cloud the function of the other leading to a more complicated diagnosis and treatment. Remarkably, as one of the injuries improves, typically improvement in the other injury becomes discovered.
Diagnosing Brain Injury
A history and physical is the first step in diagnosing a brain injury. This will include information about medical causes and trauma causes. It will include onset time and process (slow or fast), changes in medical status or sudden trauma, if consciousness was lost and if so for how long, changes in alertness, speaking, or coordination, if the head or other parts of the body (spinal cord) were injured, if there was a fall, or if the body was severely jarred or shaken.
A neurological examination including the cranial nerves (nerves of the brain), sensation and function of the body will be done. If a spinal cord injury is present, the ASIA or as it is also known the ASIA Impairment Scale (AIS) assessment will be completed to assess each level of the spinal cord. Four key factors are considered in the neurological examination for sudden onset of BI.
- Neurological Imaging–normal or abnormal
- Post traumatic amnesia (memory loss)–Differentiation is under 24 hours vs. over 24 hours of memory loss. This assessment is considered mostly with traumatic injury as those with medical causes of BI may have a gradual change in memory vs. a sudden loss as with trauma. There are instances of sudden memory loss in medical cases for example the sudden onset of stroke.
- Loss of consciousness may occur with BI. Loss of consciousness or altered levels of consciousness are rated as 0-30 minutes, greater than 30 minutes to less than 24 hours, and more than 24 hours.
- Glasgow Coma Scale score–is a measure of brain injury. Best score assessed in 24 hours, 15-13=mild brain injury, 12-9=moderate brain injury, and less than 9=severe brain injury.
Those with suspected dual diagnosis of brain injury and spinal cord injury will have an assessment of their spinal cord function. This is completed using the ASIA or AIS assessment tool. Each level of the spinal cord is assessed for sensation and movement.
Neuroimaging will be done to inspect the brain and, perhaps, the spinal cord. This includes a Magnetic Resonance Imaging scan (MRI) or Computerized Tomography (CT Scan). These tests will provide images of the brain structure, fluid or blood collection, bone fracture or displacement, blood clots, contusions, and swelling. Neuroimaging results will be normal or abnormal. Advanced imaging such as diffuse tensor imaging (DTI) might note microstructural changes such as axonal damage. Functional MRI (fMRI) has been used to map changes in the brain especially in cognitive and sensory functions. Positron emission tomography (PET) scans may show more refined details of the brain, but this is still to be determined.
Neuropsychological testing is an assessment of thinking, learning, memory, motor function, perception, problem solving, decision-making and verbal ability. A specially educated psychologist called a neuropsychologist will give you a test, typically paper and pencil or computerized, that can analyze issues, locate the area of concern in the brain and suggest treatments. The neuropsychologist will also interview you and people close to you to determine how you are dealing with issues now vs. before brain injury. This testing may be done early in the diagnosis, later or in follow ups to check progress. You will need to be well rested as testing can takes three to six hours.
If you have a medical condition, laboratory blood testing may be done to check the progression of the disease or general physical health.
Symptoms of Brain Injury
Symptoms of brain injury range from very subtle to quite noticeable. Family members are often the first to pick up the subtle clues of BI as they know the individual best. Healthcare professionals know the signs and symptoms of BI but might not catch the subtle symptoms as they might not know the mental, physical, and behavioral level of the individual prior to the onset of BI.
In the hospital or rehabilitation setting, most activities are set up in a routine or just done for the individual. For example, a person is brought their meal or taken to the dining room for lunch. Noticing that they may not remember to go on their own might not be detected because of that. Medication is brought to them. They do not need to organize their pills. There is no going to the store so handling money is not an issue. All these activities can help identify issues with BI but they are not typically done or attempted daily in a hospital setting so these issues might not be identified.
Often the symptoms of BI are so subtle that you might think you as the family member or observer is just not quite up to speed yourself and brush the issue off to your own lack of sleep or worry about the individual. The individual believes they are correct in their thinking and can convince you that you need to question yourself. This is a clue to subtle brain injury.
Not all symptoms of BI may be present in every person. An individual can have one or more symptoms of BI. Individuals with spinal cord injury may not be able to elicit the physical or sensory symptoms even if they are present. After spinal cord injury, physical and sensory symptoms may not respond to testing. Children may not have the verbal or developmental skills of adults, so behavior needs to be observed.
Symptoms of Brain Injury from Medical or Trauma Causes
Cognitive or Thinking Symptoms
- Amnesia
- Confusion
- Difficulty thinking
- Difficulty with memory
- Post-Traumatic Stress Disorder (PTSD)
- Inability to speak or to understand what is said
- Difficulty concentrating
- Difficulty understanding
- Difficulty recognizing common objects
Behavior Symptoms
- Abnormal laughing and/or crying
- Impulsivity
- Lack of restraint
- Aggression
- Irritability
- Repetition of words or actions
Mood Symptoms
- Inability to control anger
- Anxiety or Depression
- Apathy towards others and activities
- Loneliness
Physical Symptoms
Loss of consciousness for a few seconds or minutes (someone else will need to observe this by noting length of time. Individuals with loss of consciousness do not know the length of time of altered mentation or even if they were unconscious.)
- Blackouts or fainting
- Instability or stiff muscles
- Nausea or vomiting
- Dilated pupil(s), unequal pupils
- Blurred vision
- Slurred speech
- Ringing in the ears
- Headache
- Sleep disturbance
- Dizziness
- Fatigue or extreme tiredness
- Loss of smell
- Bruising around the eyes (raccoon eyes)
- Sensitivity to light
- Difficulty speaking
- Sensitivity to sound
- Seizures
- Pain
Children’s Brain Injury Symptoms–can also include adult symptoms
- Increase in crying with an inability to be consoled
- Unusual or easy irritability
- Change in nursing or eating habits
- Sad or depressed mood
- Change in ability to pay attention
- Change in sleep habits, drowsiness
- Loss of interest in favorite toys or activities
- Seizures
Assessing Brain Injury
After a brain injury, from trauma or medical causes, the individual may enter a state of coma or loss of consciousness. This can be for a short time, hours, days or longer. Methods to assess recovery are used to detect progress. Assessment scales have been developed to assess level of consciousness and recovery in a consistent manner.
Brain injury assessment scales include movement as a measure of conscious function. With a dual diagnosis of brain injury and spinal cord injury, movements may not be able to be assessed due to the SCI. Therefore, assessments are adapted accordingly. The results of the scales may not reflect the full potential of an individual with a dual diagnosis.
There are over 300 different scales to assess brain injury. The common ones are listed here. If a different scale is used, ask about the measurements and how they are assessed. Follow up assessments should be consistently made with the same scale. Ratings cannot be analyzed using different scales as the assessments and measurements are unique to each.
Glasgow Coma Scale (GCS)
The GCS was initiated in 1974 as an assessment of head injury (including brain injury) using eye movement, speaking and body movement by the individual in a coma. The assessment is performed by healthcare providers repeatedly to assess changes. The individual is observed, stimulated for a response, and then rated using this scale.
General guidelines indicate a total score of 13-15 indicates a mild head injury. A score of 9-12 is a moderate head injury. A score of 8 or less indicates a severe head injury. These scores are a general summary. The Royal College of Physicians and Surgeons of Glasgow’s website concerning the Glasgow Coma Scale contains information about how to use the scale and interpret it in detail. More precise interpretation guidelines are provided here.
The Coma Recovery Scale-Revised (also known as the JFK Scale)
The CRS-R is used to standardize assessment of neurobehavioral issues in individuals with altered levels of consciousness (coma). The scale assists with diagnosis, behavioral recovery, predicting outcomes and assesses treatment effectiveness. It notes differences in very dense levels of coma. Evaluations of hearing (auditory), sight (visual), movement (motor), mouth function (oral motor), communication and arousal are assessed. Results of the scale are between 0-23 with lower scores indicating reflex activity and high scores indicating voluntary activity.
The Coma Recovery Scale-Revised score sheet is available for review on the Shirley Ryan AbilityLab website.
Rancho Los Amigos Levels of Cognitive Functioning Scale is used to assess recovery of brain injury. It is a 10-level scale that provides indications about cognitive and behavioral abilities. The scale begins with no response at level one through to level 10 purposeful/appropriate. Sunnybrook Rehabilitation Center offers a booklet about the Rancho Los Amigos levels of cognitive functioning that includes suggestions for family and friends at each level.
The Functional Independence Measure (FIM) and Functional Assessment Measure (FAM) The FIM and FAM are the most widely used assessments in the acute care rehabilitation setting. The Functional Independence Measure consists of 18 items to assess progress in physical, psychological, and social function. The coordinating Functional Assessment Measure consists of 12 additional items to assess cognitive, behavioral, communication, and community functioning abilities. The items of these scales are assessed weekly or every other week to assess progress. The FIM and FAM assessment scales can be obtained from the Shirley Ryan AbilityLab website.
Disability Rating Scale (DRS) was developed to assess traumatic brain injury (TBI) from onset to living in the community. This 30-point scale is used to assess consciousness, cognitive ability, dependence on others and employability. It can be obtained from the Shirley Ryan AbilityLab website.
Mini Mental State Examination This is a brief screening of mental function that is typically performed in a clinical situation such as a medical office. It can easily be done in a short amount of time as a screening for cognitive impairment. If indicated, a referral is made for more definitive testing. This assessment would be used most likely if a person is living in the community when the effects of brain injury are first noted. The mini mental exam can be downloaded for free from this site.
Craig Handicap Assessment and Reporting Technique (CHART) is a 32-item assessment that is used in a community setting. It indicates issues of brain injury after discharge from the rehabilitation setting. Assessments include physical and cognitive independence, mobility, occupation, social integration, and economic self-sufficiency. A short form of 19 items also is available. The complete instruction and interpretation booklet is available from Craig Hospital.
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) was revised in 2019. It is also called the ASIA exam or AIS scale. The American Spinal Injury Association (ASIA) developed this tool that assesses sensory and motor function of each level of the spinal cord.
Treatment for Brain Injury
Treatment of brain injury should begin as soon as possible to enable the best outcomes. BI from medical causes, trauma or BI discovered later will require diagnosis and treatment. Depending on where the individual is in the progression of BI will determine their treatment needs.
Mild Brain Injury such as concussion has been traditionally treated by resting the brain. This includes reduction in physical exertion as well as less cognitive (mental) stimulation such as no TV, video games or computer use, reading or challenging work or schoolwork for a time determined by your healthcare professional. Resting the brain was thought to be calming or unchallenging so the healing process can occur. However, more recent research indicates that mild exercise can assist in recovery from concussion. Follow the treatment plan set by your healthcare professional for your unique needs.
Emergency Care Emergency care is most often required for those with traumatic brain injury. It is provided for someone with an emergency medical condition. Stabilization of the body, providing respiratory and life support, control of bleeding and blood pressure, stabilization of other injuries such as an injury to the spinal cord is a priority as is emergency surgery to control bleeding or blood clots in the brain. Skull fractures will be repaired.
Intracranial Pressure Monitoring may be needed for assessment in the acute phase of brain injury. A probe is inserted through the skull in a sterile procedure to measure the pressure inside the head. As the skull is rigid, increased pressure will force the delicate brain tissue to collapse leading to more damage if not monitored. This monitor may be left in for a period of time. Precautions are taken to ensure the best position for the individual. Visitors must not reposition the patient or change the bed height to avoid increasing pressure.
Brain Injury Treatment includes versatile approaches. Typically, medications will be used to ease issues for the individual, psychological treatment, movement, and family involvement are essentials of the treatment plan. Many healthcare specialists may be involved with your treatment plan.
Medications Typically Used for Therapeutic Treatment of Brain Injury
Not everyone with a brain injury will require medications. Individuals with certain conditions or issues may take medications. Individuals may begin medication to increase alertness and control health issues. Others may add or remove medications as needed.
- Analgesic medication reduces pain.
- Anti-anxiety medication calms feelings of confusion or processing information.
- Anticoagulants prevent blood clots.
- Anticonvulsants prevent seizures.
- Antidepressants treat symptoms of depression and mood swings.
- Antipsychotics assist with control of combativeness, hostility, hallucinations, sleep disorders.
- Diuretics remove fluid that can increase pressure inside the brain.
- Muscle relaxants reduce muscle spasms.
- Sedative-Hypnotic Agents induce sleep, mental and physical response, awareness, and pain.
- Stimulants increase alertness and attention.
Therapy for Brain Injury
Treatment for brain injury occurs in different locations depending on the need of the individual. Assessment and initiating treatment can begin in the acute care hospital. The individual may utilize rehabilitation services in an acute rehabilitation facility if the brain injury is severe or if multiple health issues are involved especially a dual diagnosis of brain injury and spinal cord injury. Brain injury from medical conditions may be initiated in a medical office. Services provided in a subacute rehabilitation center might be used for longer treatment times. Transitional care settings are a residential type of facility where services can be accessed. Day treatment centers are facilities where therapy is provided during working hours, but the individual spends the rest of the day at home. You may live at home with treatment in an outpatient clinic, medical office, or therapy center by appointment.
Cognitive Behavior Therapy (CBT) is often used in treatment of brain injury. The goals of CBT are to improve memory, attention, perception, learning, planning, and judgment. In CBT, thinking patterns are changed through learning. An individual works to recognize distortions in thinking followed by problem-solving skills to change issues with the thinking pattern. Behavioral patterns can also be modified by assessment of problematic interactions with people by using strategies to improve them. The individual learns to calm their mind and relax their body.
Neuroplasticity is a concept that one part of the nervous system can adapt for another part that is challenged. This is the idea that the nervous system is ‘plastic’ or can be molded to fit an individual’s healthcare needs. Neuroplasticity is the natural process of neurological recovery. After brain injury, activity is introduced to the body in repetitive actions which stimulates neuroplasticity. This treatment is used for physical activity such as walking, performing activities of daily living, speech skills as well as thinking skills. It takes advantage of engaging the whole brain for recovery.
Family is key to the recovery of individuals with brain injury. Recovery from brain injury is a full-time process, not just in treatment sessions. Providing support and patience is needed in recovery. Families, friends and professionals involved in the care of the individual should participate in follow-through of treatments and provide support. Family members are encouraged to maintain their own mental well-being through support groups, counseling, or family counseling so they can incorporate treatment strategies into interactions with the family member who has a brain injury.
Specialists Involved in Brain Injury Recovery and What They Provide
Most individuals who have a brain injury are treated by a team of specialists that work together to coordinate a program unique to each individual’s needs.
A Neuropsychologist is an individual specially educated in the diagnosis and treatment of brain injury. They will provide testing to pinpoint the area of the brain that has been injured followed by recommending specific treatments for improvement. They evaluate your progress to ensure you are improving and guard against setbacks.
A Neurologist is a physician that specializes in issues of the nervous system. Some further specialize in brain injury. This person will provide the ongoing medical care needed including treatments and medications for brain injury.
A Physiatrist is a physician who specializes in physical medicine and rehabilitation. They are the person who evaluates your needs for therapy and treatment for recovery. They will serve as the point person during the recovery period as well as following up long term.
A Psychological Counselor will help you learn to deal with interpersonal issues, coping skills and emotional well-being.
A Neurosurgeon is the medical specialist who will perform surgery on the brain or spinal cord to correct any structural issues that are needed to preserve life and avoid further complications and damage.
A Neuro-ophthalmologist is a specialist who understands both neurology and ophthalmology. This enables them to provide care for eye needs as related to brain injury concerns.
A Neuro-optometrist can help accommodate improved vision needed due to brain injury.
A Physical Therapist is a person who provides treatments to your body for movement, strength, balance, and energy. This specialist will help maintain your flexibility. They will coordinate your care to include treatment to other movement issues as well.
An Occupational Therapist assists with tasks of daily living such as dressing, eating, bathing, fine motor, and life skills.
The Speech Therapist assists with skills of communication, speaking, swallowing, and eating. They will also teach orientation and organization skills.
Aquatic therapy is provided to improve muscle movement, strength, coordination, ambulation, endurance, and reduce pain. This therapy is done in a warm water pool to reduce resistance of gravity and utilize buoyancy. Aquatic therapy can be very calming.
Rehabilitation Nurses assist with personal care and education of care strategies. They can teach you about your brain injury, treatments, and medications. These professionals work in various locations including your home to ensure you have the knowledge needed for daily life care.
Recreational Therapists are beneficial in finding ways to adapt your favorite activities to your specific needs.
Social Workers assist with adjustments to life. They can assist with locating resources that you may need to continue your care.
Case Managers are individuals who work with payor sources such as insurance companies to ensure you have the care and equipment needed for your situation.
Vocational Counselors assist with return to work and community living. They will provide strategies for workplace challenges.
Other health care professionals such as respiratory therapists, wound care specialists, and orthopedic surgeons will be consulted as your individual needs indicate.
Recovery from Brain Injury
Recovery from brain injury varies due to multiple factors. Early diagnosis of BI is critical for treatment to begin. Like any medical condition, the earlier treatment begins it typically results in better outcomes. Some BIs are mild, so symptoms do not appear until the individual is out of the hospital and challenged with life’s daily tasks. Symptoms may be hidden by other medical issues such as disease or spinal cord injury so that assessments are not clear. Other cases of BI are severe and readily noticeable.
Recovery from brain injury is unique to each person. No two cases are exactly alike as no two individuals are exactly alike. Predictions of recovery might be made by the treatment team but typically, progress is noted as it happens. Recovery generally follows the levels in the Rancho Los Amigos Level of Cognitive Functioning Scale presented above. Brain injury recovery does not follow a step-by-step pattern. Some individuals flow through the levels quickly, others may take a longer amount of time to get through the levels.
It is important to maintain hope, patience and keep up with therapy. Techniques learned in brain injury recovery can be used throughout the lifespan.
There are factors that can affect the diagnosis, treatment, and recovery from TBI. These are issues that should be considered in treatment planning. They are not limitations to recovery.
Age Brain injury is found at higher rates in individuals younger than 25 years and older than 75 years, with this population increasing mostly due to falls. Older individuals have greater disability with physical and cognitive function, more depression, increased hospitalizations, and mortality. Because these are known variables, treatment plans are adjusted to assist with them.
Gender BI is more prevalent in males. Historically, this has been due to occupational and lifestyle factors. Males tend to have more depression. However, as women gain in equality, gender differences are lessening. There are theories that hormonal differences could be protective in the microscopic changes in females of reproductive age in recovery.
Type of Injury Penetrating injury or open head injuries have an increased risk of complications and death mostly due to infection. They are associated with increased pneumonia, skull fracture, cerebrospinal fluid leak and hypotonia (poor muscle tone). Blast injuries have higher rates of sensory deficits, pain, and multi-trauma. Dual diagnosis of BI and spinal cord injury can complicate recovery due to issues in the brain and spinal cord. They can compound recovery factors.
Genetics More recent studies indicate genetics play a part in recovery of BI although there is more that needs to be researched in this area. Using genetic studies of individuals with dementia and other neurodegeneration diseases such as Alzheimer’s, apolipoproteinE (ApoE), a lipid transport protein, may be protective in BI recovery.
Access to Care Individuals with less access to diagnostic and ongoing treatment have poorer outcomes. Those without insurance have shorter hospital stays and less access to rehabilitation facilities and treatments. Those that live in rural areas with less access to neuroimaging for diagnosis and therapies for rehabilitation also had poorer outcomes.
Lack of Reporting Some individuals or family members do not report changes in abilities. This can be from embarrassment, stigma, fear, lack of knowledge about BI or an unawareness that treatments are possible. Individuals with mild symptoms may wait for them to resolve on their own. Symptoms can be subtle and written off to a poor night’s sleep or other excuses. Any changes should be reported to your healthcare professional for investigation and treatment.
Brain Injury Facts and Figures
Facts about Brain Injury focus on Traumatic Brain Injury (TBI). Acquired Brain Injury (ABI) is typically listed in the diagnostic group such as stroke, anoxia (lack of oxygen to the brain), tumors, etc.
The number of TBIs occurring annually is 2.5 million.
Causes are falls (35%), motor vehicle accidents (17%), and being struck by or against something (16%).
Individuals who have a disability from brain injury number 80,000 to 90,000 per year.
Currently there are 3.1 million individuals living in the U.S. with disabilities from brain injury.
Research
Research about brain injury is extensive. Information from the assessment instruments is studied to determine treatments that are effective. There are many major programs, governmental agencies and the U.S. government that sponsor and conduct extensive research projects in all aspects of brain injury. You will see quite a few of the treatments for brain injury are the same as for spinal cord injury because the nervous system acts as a unit.
Stem cells are being studied for effectiveness in brain recovery at a molecular level. Currently, these studies are being conducted in the laboratory with extremely few conducted with humans. However, the results are leading to a hopeful outcome for people.
Virtual reality is being studied in all areas of rehabilitation, including brain injury. This process involves computer simulations and other robotics such as weight supported walking. The information being gathered has been and continues to evolve with improvements in successful outcomes for individuals with brain injury.
Activity based rehabilitation strategies that include patterned movement has been demonstrated as successful to provide input to the healing brain. This research continues with many therapies including aquatics and weight supported walking that are in use today.
Fatigue is an issue for individuals with spinal cord injury. Research of this phenomena and how to treat it is being conducted including physiologic studies, medications, and therapies.
Electromagnetic brain stimulation is demonstrating effectiveness in the laboratory setting. Initial studies of cortical stimulation in combination with existing and advanced therapeutic treatments is resulting in improved outcomes. These studies are in early phases.
To learn more about brain injury research, the National Institute of Neurological Disorders and Stroke provides information about studies.
The United States government registry of clinical trials can be found here.
Consumer Resources
If you are looking for more information about brain injury or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm ET.
Additionally, the Reeve Foundation maintains a fact sheet about brain injury with additional resources from trusted Reeve Foundation sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to brain injury (BI) support groups and organizations, including:
Brain Injury Association of America
Centers for Disease Control and Prevention (CDC):
https://www.cdc.gov/traumaticbraininjury/get_the_facts.html
https://www.christopherreeve.org/wp-content/uploads/2024/04/TBI_Clinicians_Factsheet-a.pdf
https://www.christopherreeve.org/wp-content/uploads/2024/04/TBI_Patient_Instructions-a.pdf
Rancho Los Amigos National Rehabilitation Hospital
Traumatic Brain Injury Center of Excellence (formerly called Defense and Veterans Brain Injury Center) TBICoE serves military personnel and veterans.
References
Beaulieu CL, Dijkers MP, Barrett RS, Horn SD, Giuffrida CG, Timpson ML, Carroll DM, Smout RJ, Hammond FM. Occupational, physical, and speech therapy treatment activities during inpatient rehabilitation for traumatic brain injury. Arch Phys Med Rehabil. 2015 Aug;96(8 Suppl):S222-34.e17. doi: 10.1016/j.apmr.2014.10.028. PMID: 26212399; PMCID: PMC4538942.
Bogdanova Y, Yee MK, Ho VT, Cicerone KD. Computerized cognitive rehabilitation of attention and executive function in acquired brain injury: A systematic review. J Head Trauma Rehabil. 2016 Nov/Dec;31(6):419-433. doi: 10.1097/HTR.0000000000000203. PMID: 26709580; PMCID: PMC5401713.
Brotfain E, Gruenbaum SE, Boyko M, Kutz R, Zlotnik A, Klein M. Neuroprotection by estrogen and progesterone in traumatic brain injury and spinal cord injury. Curr Neuropharmacol. 2016;14(6):641-53. doi: 10.2174/1570159×14666160309123554. PMID: 26955967; PMCID: PMC4981744.
Cipriano CA, Pill SG, Keenan MA. Heterotopic ossification following traumatic brain injury and spinal cord injury. Journal of the American Academy of Orthopaedic Surgeons. November 2009 – Volume 17 – Issue 11 – p 689-697. https://journals.lww.com/jaaos/fulltext/2009/11000/heterotopic_ossification_following_traumatic_brain.3.aspx
Dang B, Chen W, He W, Chen G. Rehabilitation treatment and progress of traumatic brain injury dysfunction. Neural Plast. 2017;2017:1582182. doi: 10.1155/2017/1582182. Epub 2017 Apr 11. PMID: 28491478; PMCID: PMC5405588.
Heled E, Tal K, Zeilig G. (2020) Does lack of brain injury mean lack of cognitive impairment in traumatic spinal cord injury? J Spinal Cord Med., DOI: 10.1080/10790268.2020.1847564
Galgano M, Toshkezi G, Qiu X, Russell T, Chin L, Zhao LR. Traumatic brain injury: Current treatment strategies and future endeavors. Cell Transplant. 2017 Jul;26(7):1118-1130. doi: 10.1177/0963689717714102. PMID: 28933211; PMCID: PMC5657730.
Garlanger KL, Beck LA, Cheville AL. Functional outcomes in patients with co-occurring traumatic brain injury and spinal cord injury from an inpatient rehabilitation facility’s perspective. J Spinal Cord Med. 2018 Nov;41(6):718-730. doi: 10.1080/10790268.2018.1465744. Epub 2018 May 1. PMID: 29714644; PMCID: PMC6217473.
Gerrard, Paul B et al. “Coma Recovery Scale-Revised: evidentiary support for hierarchical grading of level of consciousness.” Arch Phys Med Rehabil. 95 12 (2014): 2335-41.
Giacino JT, Fins JJ, Laureys S, Schiff ND. Disorders of consciousness after acquired brain injury: the state of the science. Nat Rev Neurol. 2014 Feb;10(2):99-114. doi: 10.1038/nrneurol.2013.279. Epub 2014 Jan 28. PMID: 24468878.
Houlden H, Greenwood R. Apolipoprotein E4 and traumatic brain injury. J Neurol Neurosurg Psychiatry. 2006 Oct;77(10):1106-7. doi: 10.1136/jnnp.2006.095513. Epub 2006 Jun 22. PMID: 16793859; PMCID: PMC2077546.
Jonasson A, Levin C, Renfors M, Strandberg S, Johansson B. Mental fatigue and impaired cognitive function after an acquired brain injury. Brain Behav. 2018 Aug;8(8):e01056. doi: 10.1002/brb3.1056. Epub 2018 Jun 29. PMID: 29956894; PMCID: PMC6085903.
Karnath HO, Sperber C, Rorden C. Mapping human brain lesions and their functional consequences. Neuroimage. 2018 Jan 15;165:180-189. doi: 10.1016/j.neuroimage.2017.10.028. Epub 2017 Oct 16. PMID: 29042216; PMCID: PMC5777219.
Kushner DS. Strategies to avoid a missed diagnosis of co-occurring concussion in post-acute patients having a spinal cord injury. Neural Regen Res. 2015 Jun;10(6):859-61. doi: 10.4103/1673-5374.158329. PMID: 26199589; PMCID: PMC4498334.
Leddy JJ, Wilber CG, Willer BS. Active recovery from concussion. Curr Opin Neurol. 2018 Dec;31(6):681-686. doi: 10.1097/WCO.0000000000000611. PMID: 30382949; PMCID: PMC7046089.
Macfarlane RJ, Ng BH, Gamie Z, El Masry MA, Velonis S, Schizas C, Tsiridis E. Pharmacological treatment of heterotopic ossification following hip and acetabular surgery. Expert Opin Pharmacother. 2008 Apr;9(5):767-86. doi: 10.1517/14656566.9.5.767. PMID: 18345954.
Mckee AC, Daneshvar DH. The neuropathology of traumatic brain injury. Handb Clin Neurol. 2015;127:45-66. doi: 10.1016/B978-0-444-52892-6.00004-0. PMID: 25702209; PMCID: PMC4694720.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on the Review of the Department of Veterans Affairs Examinations for Traumatic Brain Injury. Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans. Washington (DC): National Academies Press (US); 2019 Apr 10. Diagnosis and Assessment of Traumatic Brain Injury. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542595/
Nott MT, Baguley IJ, Heriseanu R, Weber G, Middleton JW, Meares S, Batchelor J, Jones A, Boyle CL, Chilko S. Effects of concomitant spinal cord injury and brain injury on medical and functional outcomes and community participation. Top Spinal Cord Inj Rehabil. 2014 Summer;20(3):225-35. doi: 10.1310/sci2003-225. PMID: 25484568; PMCID: PMC4257139.
Pessoa L. A Network Model of the Emotional Brain. Trends Cogn Sci. 2017 May;21(5):357-371. doi: 10.1016/j.tics.2017.03.002. Epub 2017 Mar 28. PMID: 28363681; PMCID: PMC5534266.
Polinder S, Cnossen MC, Real RGL, Covic A, Gorbunova A, Voormolen DC, Master CL, Haagsma JA, Diaz-Arrastia R, von Steinbuechel N. A multidimensional approach to post-concussion symptoms in mild traumatic brain injury. Front Neurol. 2018 Dec 19;9:1113. doi: 10.3389/fneur.2018.01113. PMID: 30619066; PMCID: PMC6306025.
Silva MA, See AP, Essayed WI, Golby AJ, Tie Y. Challenges and techniques for presurgical brain mapping with functional MRI. Neuroimage Clin. 2017 Dec 6;17:794-803. doi: 10.1016/j.nicl.2017.12.008. PMID: 29270359; PMCID: PMC5735325.
Simpson G, Jones K. How important is resilience among family members supporting relatives with traumatic brain injury or spinal cord injury? September 2012 Clinical Rehabilitation 27(4). DOI: 10.1177/0269215512457961
Snyder AZ, Bauer AQ. Mapping structure-function relationships in the brain. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019 Jun;4(6):510-521. doi: 10.1016/j.bpsc.2018.10.005. Epub 2018 Oct 29. PMID: 30528965; PMCID: PMC6488459.
Stillman A, Alexander M, Mannix R, Madigan N, Pascual-Leone A, Meehan WP. Concussion: Evaluation and management. Cleve Clin J Med. 2017 Aug;84(8):623-630. doi: 10.3949/ccjm.84a.16013. PMID: 28806161.

