Arteriovenous Malformations
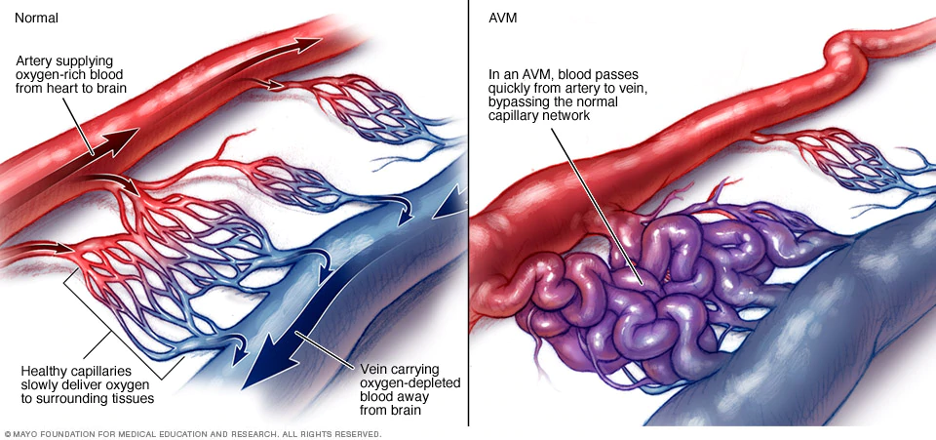
In the body’s circulation, arteries deliver enriched blood to the cells. Body cells obtain the enriched blood through capillaries. Veins carry blood and waste products away from the cells. Very rarely, an artery may connect directly to a vein bypassing the capillaries which are missing. This missed step results in an arteriovenous (artery to vein) malformation (AVM). An AVM is often described as a ‘tangled web’ of vessels at the location of miscommunicated blood flow.
The area of the misconnection causes the blood vessel to dilate due to rapid blood flow through the artery which is not slowed by the capillaries. Over time, the walls of the blood vessels become thin and weak, leading to possible rupture. The result of the AVM is bleeding into tissue of the body.
AVMs can occur in any part of the body. In many cases, an AVM might be present but never ruptures. People do not ever know it is there. Some AVMs rupture in parts of the body that can accommodate some extra fluid in the tissue until it is absorbed.
An AVM in the Central Nervous System (CNS) is a serious condition. If an AVM in the spinal cord or brain ruptures, there is no room for even a small amount of extra blood because the spinal cord is surrounded by bony vertebrae that do not expand. The brain is surrounded by the skull that also does not allow for expansion. The extra blood in the CNS will push on healthy nerve tissue depriving the spinal cord or brain of oxygenated blood flow. Due to the pressure of the extra blood pressing on the soft neurological tissue, a change in blood pressure at the site and bleeding into the surrounding neurological tissue results in damage to the spinal cord or brain.
An AVM in the spinal cord is designated as a spinal AVM. It is abbreviated as sAVM. Since sAVM in the spinal cord or AVM in the brain is a hemorrhage (bleeding) into tissue it is considered a type of hemorrhagic stroke. Strokes can occur in the Central Nervous Systems which includes both the spinal cord and brain.
Nervous tissue damage creates functional deficits. How your body is affected depends on the location of the bleed as well as the amount of bleeding that occurs. For example, you can have an sAVM bleed in the spinal cord where there is a significant nerve that is affected, or you can have a great deal of bleeding that affects many nerves in the spinal cord and extends into the brain.
Some AVMs rebleed. The risks for a second rupture of an AVM include when the AVM presents with hemorrhage, when there is deep venous drainage, when associated with an aneurysm, or when in a deep location.
The cause of a sAVM or other AVM is unknown. At one time AVMs were thought to be a congenital abnormality meaning they occur during development of the fetus. This theory is being challenged. Current theories about AVM formation are that they are genetic or have a family tendency. Still others think they may be due to some neurological event like an undetected, small stroke.
sAVM in the pediatric population is rarer than in adults. This might be due to the elasticity of children’s blood vessels. Surgical correction of a pediatric sAVM has lower consequences than with adults.
Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved.
Types of AVM
AVMs can occur anywhere in the body. When an AVM occurs in the spinal cord or brain, the consequences can be significant.
In the spine
sAVMs were categorized in four groups by Anson and Spetzler in 1992.
Type 1 is an sAVM of the dura (covering of the spinal cord) at the nerve root sleeve. These result in poor blood flow to the spinal cord. This is the most common sAVM, appearing typically in individuals older than 40 years and more often in men.
Type 2 is intradural (inside the covering of the spinal cord) inside a short segment of the spinal cord. These occur most often in individuals less than 30 years old.
Type 3 is an sAVM in the spinal cord tissue that are fed by multiple blood vessels. They typically occur in individuals less than 30 years old.
Type 4 is an sAVM on the surface of the spinal cord.
Ages are approximate. You could have an sAVM and be out of the typical age range for that type.
In the brain
True arteriovenous malformation (AVM)-The most common brain vascular malformation. The blood vessels are connected without brain tissue in between the artery and the vein. It looks like a web of blood vessels.
Occult or cryptic AVM or cavernous malformations–A small AVM that bleeds a very small amount. It may produce seizures.
Venous malformation–A malformation only of the veins
Hemangioma–Malformed blood vessels found on the surface of the brain and on the skin or face.
Dural fistula–Occurs in the covering (dura) of the brain. Can be behind the eye, ear, or top of the head.
Symptoms of sAVM
In the Spine
Sudden and severe pain in the back, usually at the level of the AVM
Loss of movement and/or sensation, numbness, tingling, stiffness
Loss of coordination, balance
Incontinence or difficulty with urine and/or bowel elimination
If the bleeding from an sAVM is extensive, the blood will extend into the area of least pressure which is into the brain. Therefore, it is important to know the symptoms of a brain AVM as well. Symptoms of a sAVM may first appear in the brain.
In the Brain
- Localized headache
- Seizures
- Loss of movement and or sensation to all or parts of the body, numbness, tingling
- Loss of coordination
- Changes in vision
- Loss of speech or slurring of speech
- Difficulty planning tasks
- Dizziness
- Mental confusion
- Hallucinations or dementia
Diagnosing AVM
A physical examination including a neurological examination is performed. You will be asked about the specifics of the event. This information will lead the healthcare professional to obtain further testing for sAVM.
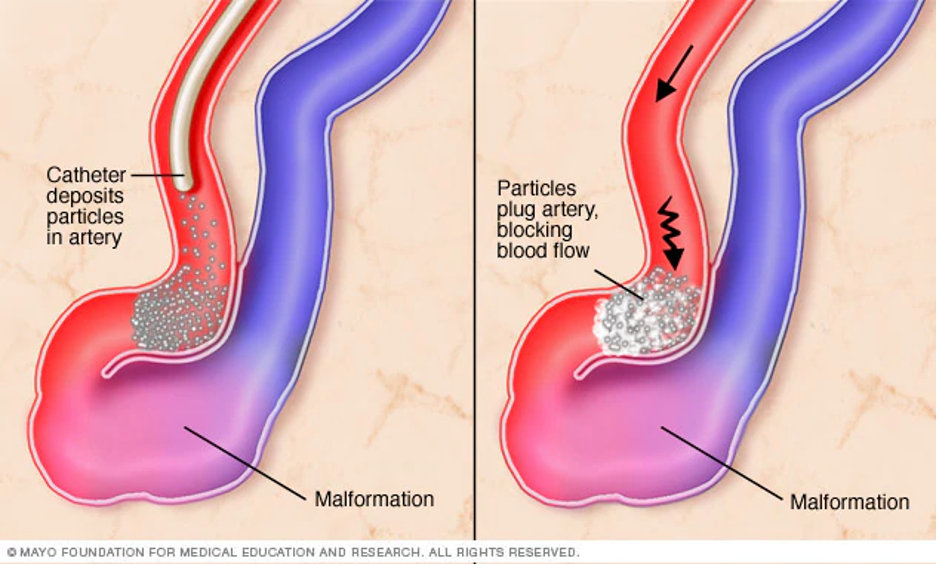
AVMs are visualized by a healthcare professional for diagnosis. An MRI (magnetic resonance imaging) spinal scan might be performed to help identify the sAVM. X-ray angiography is needed for a specific diagnosis. In this test, a very small catheter is inserted into a blood vessel in the groin and threaded to the location of the AVM. The blood flow system is then studied.
Treatment for AVM
Some individuals have an sAVM but never know it exists. Some sAVMS are found while receiving treatment for something completely different. For instance, you might have a spinal scan for a ‘pulled muscle’ but an sAVM might be noticed on the scan. Treatment depends on the size and location of the sAVM. If the sAVM is in a location that would create more damage to treat, it might be monitored or treated conservatively.
The goal for treatment is to prevent the sAVM from bleeding or rebleeding. Conservative treatment includes avoiding strenuous exercise and blood thinning medication. If surgery is planned, you will be asked to follow these instructions until the time of the surgery. It is also wise to avoid straining with toileting or other activities.
Most sAVMs are diagnosed after a bleed. There are three options of surgical procedures that are used to treat sAVMs. The choice of type of surgery depends on the location of the sAVM. General neurosurgery starting with a laminectomy is one option. For more complicated locations, either stereotactic radiosurgery or interventional neuroradiology/endovascular neurosurgery is performed. Stereotactic radiosurgery is done by use of a focused high energy beam to scar and clot the sAVM. In interventional neuroradiology/endovascular neurosurgery a small catheter is threaded into the sAVM where it is then sealed off.
Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved.
Recovery From AVM
Some individuals have surgery to repair their sAVM without complications. Others might have some issues that remain from the sAVM bleed or as a consequence of the surgery to correct it.
After the sAVM is contained, functional issues can remain. These are the result of pressure on the nervous tissue of the spine and even the brain if bleeding extended that far. The residual issues are considered to be a spinal cord injury (SCI). The SCI is evaluated using the AIS assessment. Each level of the spinal cord will be tested for function and sensation. A complete injury indicates no messages are getting through to the end of the spinal cord. An incomplete injury is some messages are transmitted through the spinal cord although not completely. The level of injury is the last completely functioning spinal cord segment. More detail of a spinal cord assessment is located in the spinal cord injury section:
Rehabilitation
Recovery from sAVM takes some time. Physical rehabilitation will be provided to help you learn to function in your current status with the goal of long-term improvements. A physiatrist (an M.D. with a specialty in rehabilitation medicine) is typically the leader of the team. This could also be another healthcare professional with extensive physical rehabilitation experience.
A Physical Therapist (PT) will work with you to improve your strength, locating your body in space and gross motor skills. They will begin with evaluating you at your current level. The goal will be to improve mobility and function from wheelchair use to walking depending on the type and level of injury.
An Occupational Therapist (OT) will help you to improve your activities of daily living such as dressing, bathing, and feeding. The OT will help you to improve your fine motor skills.
A Speech-Language Pathologist (SLP) will work with you if you have affects to your cognition or other brain issues. This professional will help you with orientation, thinking, speaking and swallowing as necessary.
The Rehabilitation Nurse will help coordinate your care in the rehabilitation setting as well as in the transition to home. The nurse will teach you to manage your bowel, bladder and skin care needs as well as medications, diet and other health care education.
A Psychologist might be assigned to your team to help you adjust to changes in your life.
Others on the team might include a social worker, dietician, vocational counselor as well as other medical professionals for specific issues you may have.
Clinical practice guidelines are developed plans for care of individuals with specialty needs. After an sAVM, the guidelines used for rehabilitation are for spinal cord injury. Clinical practice guidelines are available to model standards for healthcare professionals and the public about rehabilitation strategies.
The Paralyzed Veterans of America (PVA) organization has a wide variety of evidence-based guidelines available free of charge. https://pva.org/research-resources/publications/clinical-practice-guidelines/
The American College of Physicians develops guidelines and reccomendations on various topics. https://www.acponline.org/clinical-information/guidelines
The American Academy of Physical Medicine and Rehabilitation provides a wide array of information at their website. https://www.aapmr.org/home
Research
Research of AVMs is very active. Researchers are looking at the source of AVMs. They are attempting to differentiate if they develop in the fetal stage, the genetics links, or if there is a cause that is yet unknown. Once a cause or the source of a problem is understood, methods to prevent and treat it can be developed.
Another line of research is to determine if and when AVMs should be surgically treated. The investigators are attempting to look at outcomes, especially mortality, to see if surgery should be attempted or not. Much of this depends on the location of the sAVM.
There are various types of surgical techniques that can be used to treat sAVMs. Each of these techniques are being investigated for outcomes to match the best treatment plan for each type of sAVM.
Long term effects of sAVMs are being studied extensively through the research into spinal cord injury in prevention and reduction of secondary conditions. All causes of SCI are under investigation including medical causes and trauma. Research of the physiology of SCI affects medical causes and trauma.
Research studies are listed on the government site: https://clinicaltrials.gov/.
Since AVM is a rare disorder, research studies are also listed on the National Organization for Rare Disorders (NORD) website: https://rarediseases.org/for-patients-and-families/information-resources/news-patient-recruitment/
sAVM Facts and Figures
AVM is more common in men than in women.
Occurrence of sAVM is less than 3% of the population which makes AVM a very rare condition.
The average age for sAVM diagnosis is about 30-45 years but can occur at any time in the lifespan.
The most common sAVM is intradural (inside the spinal cord covering) at 80%.
Consumer Resources
If you are looking for more information on AVM or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm ET.
Additionally, the Reeve Foundation maintains a fact sheet on arteriovenous malformations with additional resources from trusted Reeve Foundation sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to Arteriovenous Malformation (AVM) support groups and organizations, including:
Aneurysm and AVM Foundation https://www.taafonline.org/ (brain AVM, only)
Society of Vascular and Interventional Neurology https://www.svin.org/i4a/pages/index.cfm?pageid=3316
Additional information about sAVM can be found at these sites:
American Association of Neurological Surgeons https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Arteriovenous-Malformations
American Stroke Association https://www.stroke.org/en/about-stroke/types-of-stroke/hemorrhagic-strokes-bleeds/what-is-an-arteriovenous-malformation
National Organization of Rare Disorders https://rarediseases.org/rare-diseases/arteriovenous-malformation/
Further Reading
References
sAVM
Ozpinar A, Weiner GM, Ducruet AF. Epidemiology, clinical presentation, diagnostic evaluation, and prognosis of spinal arteriovenous malformations. Handb Clin Neurol. 2017;143:145-152. doi: 10.1016/B978-0-444-63640-9.00014-X.
Anson, J.A. and Spetzler, R.F. Classification of spinal arteriovenous malformations and implications for treatment. BNI 1992;Quarterly, 8, 2-8.
Symptoms, Treatment and Research
Brinjikji W, Lanzino G, Endovascular treatment of spinal arteriovenous malformations. Handb Clin Neurol. 2017;143:161-174. doi: 10.1016/B978-0-444-63640-9.00016-3.PMID: 28552139
Collin A, Labeyrie MA, Lenck S, Zetchi A, Aymard A, Saint-Maurice JP, Civelli V, Houdart E.J Long term follow-up of endovascular management of spinal cord arteriovenous malformations with emphasis on particle embolization. Neurointerv Surg. 2018 Dec;10(12):1183-1186. doi: 10.1136/neurintsurg-2018-014016. Epub 2018 Jul 3.PMID: 29970619
Hida K, Abe H, Iwasaki Y, Yoshimi C, Matsuzawa H, Miyasaka K. Treatment and prognosis of spinal AVM. No Shinkei Geka. 1993 Aug;21(8):711-6. PMID: 8361569
Horton JA, Latchaw RE, Gold LH, Pang D. Embolization of intramedullary arteriovenous malformations of the spinal cord. AJNR Am J Neuroradiol. 1986 Jan-Feb;7(1):113-8. PMID: 3082126
Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery. 2010 Apr;66(4):702-13; discussion 713. doi: 10.1227/01.NEU.0000367555.16733.E1. PubMed PMID: 20190666; PubMed Central PMCID: PMC2847513.
Ozpinar A, Weiner GM, Ducruet AF. Epidemiology, clinical presentation, diagnostic evaluation, and prognosis of spinal arteriovenous malformations. Handb Clin Neurol. 2017;143:145-152. doi: 10.1016/B978-0-444-63640-9.00014-X.
Rangel-Castilla L, Russin JJ, Zaidi HA, Martinez-Del-Campo E, Park MS, Albuquerque FC, McDougall CG, Nakaji P, Spetzler RF. Contemporary management of spinal AVFs and AVMs: lessons learned from 110 cases. Neurosurg Focus. 2014 Sep;37(3):E14. doi: 10.3171/2014.7.FOCUS14236. PMID: 25175433
Velat GJ, Chang SW, Abla AA, Albuquerque FC, McDougall CG, Spetzler RF. Microsurgical management of glomus spinal arteriovenous malformations: pial resection technique: Clinical article.J Neurosurg Spine. 2012 Jun;16(6):523-31. doi: 10.3171/2012.3.SPINE11982. Epub 2012 Apr 6.PMID: 22482421
Veznedaroglu E, Nelson PK, Jabbour PM, Rosenwasser RH. Endovascular treatment of spinal cord arteriovenous malformations. Neurosurgery. 2006 Nov;59(5 Suppl 3):S202-9; discussion S3-13. doi: 10.1227/01.NEU.0000237409.28906.96.PMID: 17053604

