Aging With Paralysis and Aging Into Paralysis
Aging is a natural process. Many individuals develop health conditions related to aging in later years. Paralysis can affect the aging process in different ways. If you have paralysis earlier in life, you are aging with paralysis. Those who develop paralysis later in life are aging into paralysis.

Individual age differently. Both internal and external factors affect the process. Paralysis is just one of the issues that affect how you age. Those who have paralysis earlier in life may age differently from those without paralysis. Those who develop paralysis later in life may face a compounding of challenges.
The age of 40 years is the typical time when individuals begin to experience aging. Those born with paralysis, children, teens, and young adults, or those who acquire paralysis when young, are in the group of aging with paralysis. Younger individuals usually have more options for care, have fewer acquired health issues, and have more support from family members. They are aging into paralysis.
Those over the age of 40 may develop paralysis from disease progression or injury. These individuals may not have the options of younger individuals, including where they live or continued work opportunities. Existing health conditions may already exist. Their family members may not have the physical or mental health needed to assist with care.
Younger individuals may develop secondary conditions of paralysis earlier. This includes bone density loss, decreased muscle mass, diabetes, hormonal changes, pressure injury, weight loss or gain, and cardiac issues, among others. Older individuals may develop these same issues but are compounded by the natural aging process already taking place.
Those who have paralysis at a younger age often have more resilience to combat health issues and secondary complications due to body resilience. Those who become paralyzed at an older age, with the aging process already in effect, may not have as much resilience to deal physically or mentally with the changes. However, everyone ages differently. Bodies and minds react differently. Caring for your body as you age is critical to the aging process.
This does not mean that you cannot age well with paralysis. Preparation and knowing what to do will assist you with a smoother lifestyle.
What are the Symptoms of Aging with Paralysis
Aging with paralysis: At a younger age, establishing a habit of prevention and interventions immediately can assist with decreasing the incidence and severity of health issues at an older age.
Aging into paralysis: If paralysis occurs at an older age, prevention and interventions should be followed fully to avoid a quicker onset and increased severity of health issues.
Many issues occur with paralysis that are challenging. The following is an overview of aging issues with paralysis arranged by body system, with prevention and intervention measures.
Integumentary System (Skin)
Skin is more resilient at a younger age. It is the major protective barrier of the body from outside forces, has sensation and assists with temperature regulation. In extreme cold or hot temperatures as well as with natural aging, the skin tends to become thinner and drier. Skin can become looser due to underlying muscle loss. These same changes happen more frequently in individuals with paralysis. Paralysis that occurs at a younger age can cause skin changes to occur earlier. Paralysis starting at a senior age can advance these issues more quickly.
| Skin Changes with Aging and Paralysis | Prevention | Interventions |
| Dry, flaky skin, calluses Occurs with aging, risks increase with paralysis. | Wash with warm (not hot) water, use emollient lotion, do not peel off dry skin-it leaves small openings for infection. | Slowly remove loose skin or calluses by soaking in warm water, then rub the area with a damp washcloth. This will take several attempts. Do not try to remove a callus at one time, the skin beneath the callus is tender and will break open. Give the skin under a callus time to gradually return to normal before adding pressure. Use emollient lotion. |
| Pressure Injury, Shearing, Friction rubs Can occur at any time with paralysis; risk increases with normal aging. | Perform pressure releases. Check your skin for changes in pigmentation. Lift your body fully when transferring to prevent drag on the skin. Stop smoking and alcohol, which rob the skin of nutrients. Use sunscreen and lip balm, wear a ventilated wide brimmed hat. Always use medical-grade pressure-dispersing equipment. Stay off the area with a pigment change until the spot resolves, take rest times during the day to keep off pressure points. | A change in pigment is your body telling you to remove all pressure from that area until the pigment change resolves to your normal tone. If a pressure injury occurs, follow instructions from your healthcare professional for healing. Stay off the injured area. |
| Temperature Regulation Skin senses temperature to alert the nervous system so the body adjusts to the environment to keep a healthy internal temperature. Younger individuals have slightly higher body temperatures due to activity. Older individuals may have slightly lower body temperatures due to a slower metabolism leading to feeling cold. | Dress for the weather, even if you do not feel heat or cold, your body will respond to it. Use cooling towels, fans, hats with wide brims, and shade in warm weather. In cold weather, dress in layers, on all parts of your body. Preheat or precool a vehicle before use. | Monitor for signs of overheating or overcooling of the body. Note areas where air conditioning is available in hot weather. Seek balanced heat in cold weather. Stay out of drafts. |
| Infection Skin is a barrier to keeping out germs. Younger individuals generally have a quicker response to infection. Older individuals may take time to respond. | Practice good hand and body hygiene. Monitor body positioning and transfer safety to avoid injury. | Gently clean open areas. Cover open areas with a sterile dressing. Seek medical advice for large wounds. |
| Detailed skin care information can be found here. | ||
Skeletal System (Bones)
Bones are very strong as they support the entire body structure. If a force is applied to bones that is stronger, they can break. With aging, bones can become more fragile due to decreased bone calcium levels. At any age, osteoporosis is a common complication with paralysis due to the bones not bearing weight to keep them strong. Loss of bone density occurs almost immediately after paralysis. It is also a common issue in natural aging. The risk of osteoporosis is higher in younger individuals but even higher in individuals who develop paralysis later in life.
| Skeletal Changes with Aging and Paralysis (Bones) | Prevention | Interventions |
| Osteopenia and osteoporosis are a loss of bone density. Occurs with hormonal changes in aging women and men. Paralysis increases the risk in all ages and genders of individuals within weeks due to lack of weight bearing. | Exercise and stretching the muscles either under your own power or with someone doing it for you. Standing frame use, building up to one hour per day. Careful limb handling, and placement. | Bone density testing. Treatment for osteopenia and osteoporosis |
| Fragility fractures and broken bones Usually from loss of calcium in the bones from paralysis, risk can increase with age unless bone density testing and treatment are followed | Use careful limb handling and placement. Check the positioning of the body to ensure a body part has not fallen off placement equipment. | Seek immediate treatment for injured bones. Casting or surgery will be needed. May trigger autonomic dysreflexia episodes. May have no pain, pain or referred pain. |
| Arthritis Most often occurs in older age but can appear at any time with paralysis (example, overuse of shoulders for movement). | Gently perform range of motion exercises and stretching, especially to the areas of the body with paralysis. | Medications can assist with pain control (you may not sense pain, but your body will still react to it). |
| Joint overuse Occurs at any time with paralysis from lifting your body with your arms (especially shoulders) or moving your body with braces or other movement equipment. | Handle all your joints with care. Monitor your use of adaptive equipment. Use lifting/transfer equipment, such as a sliding board, if available to you. It may become more available with aging. | Give your body time to rest after exercise. You may not feel your body reacting to hours of brace walking, FES stimulation, or use of other equipment, but your body will react to it. Can result in overuse syndromes. |
| Heterotopic Ossification (HO) HO is when bone cells grow into muscles and soft tissues. Though rare, HO can appear at any time after paralysis. | Provide range of motion to all joints. Note if the joint has less movement. | Medication can be taken to slow or eliminate the meandering bone cells. Surgical removal of the excess bone cells may be needed. |
Muscular System (Muscles)
The muscles provide movement of the body. They are in pairs, one set for pushing away is a companion to another set that pulls toward the body. The muscles that pull toward the body are just a little stronger which is why after paralysis, some individuals have limbs that draw into the body called contractures. With aging muscles may become a bit smaller and weaker. Using your muscles and exercising paralyzed muscles assist with keeping them stronger.
| Muscle changes with Aging and Paralysis | Prevention | Intervention |
| Smaller muscles Occurs at any time after paralysis, muscles crave movement even if you cannot sense it. | Exercise your body or have someone move your body. Perform pressure releases. | Electrical stimulation can assist muscle building in higher-level injuries. |
| Contractures Occur at any time after paralysis, risk may increase with age as muscle become slightly smaller. | Gentle movement of all joints can help prevent joints from becoming immobile. | More aggressive therapy may be needed to release the contracture. Slowly releasing the contracture with bracing may be necessary or even surgery. |
| Temperature Regulation Skin senses temperature to alert the nervous system so the body adjusts to the environment to keep a healthy internal temperature. | Dress for the weather, even if you do not feel heat or cold, your body will respond to it. Use cooling towels, fans, hats with wide brims, and shade in warm weather. In cold weather, dress in layers, on all parts of your body. Preheat or precool a vehicle before use. | Monitor for signs of overheating or overcooling of the body. Note areas where air conditioning is available in hot weather. Seek balanced heat in cold weather. Stay out of drafts. |
Nervous System (Nerves)
The nervous system consists of the central nervous system (the brain and spine) and the peripheral nervous system (all the other nerves in the body). The brain controls all body activities. The spinal cord carries the messages to and from the peripheral nervous system to act or to slowdown. The nervous system controls movements that you can see such as standing, toileting, and blinking. It also controls activities that you cannot see such as thinking, breathing, liver function, controlling infection, and body temperature, etc.
With paralysis, messages about temperature regulation of the body, reflexes, or infections may not be as quick as prior to paralysis or may not respond at all. This slow response can be compounded by age. Muscles may not be able to signal to the brain that the body needs to stretch which can lead to increased tone (spasticity) or contractures. Pain messages may be scrambled which can lead to neuropathic pain. Pain messages can also be slowed with age which compounds the issue.
Thinking issues can be noted with paralysis from neurological disease, head injury, or stroke. It can be an under diagnosed issue with spinal cord injury. Changes in mental status may or may not be noted by the individual but is often noted by family or caregivers at home. This could be just a slight loss of thought or more noticeable. Treatments and therapies can assist with thinking issues.
Some individuals with neurological disease, brain injury or stroke, may develop symptoms of dementia which can be compounded with aging. Noticing these symptoms can be assisted with interventions.
| Nerve changes with Aging and Paralysis | Prevention | Intervention |
| Tone (spasticity) Signaling of messages to and from the brain are unable to be transmitted successfully. A tightening of muscles. | Gentle movement of all joints helps relax mild tone due to stimulation of the muscle. | Medications can assist with relaxation of the muscles. Keep the body in good alignment to avoid contracture issues. Use non-medication techniques as well. |
| Neurogenic Pain Pain due to mis-signaling of messages. Younger individuals may be more sensitive to pain. Older individuals may have decreased pain sensations. | Maintain a positive outlook. Use distraction techniques. Treat neurogenic pain with pain medication for treatment of neurogenic pain. Opioids do not treat neurogenic pain. | Neurogenic pain medications include low-dose antiepileptic and antiseizure medications, gabapentin, and pregabalin. Use alternative therapies to avoid pain medication or to supplement pain medication. |
| Infection Control The inability of the body to recognize germs and bacteria, a slowness of recognition, or a misinterpretation of infection. | Practice good hand and body hygiene. Monitor body positioning and transfer safety to avoid injury. | Gently clean open areas. Cover open areas with a sterile dressing. Seek medical advice for large wounds. |
| Thinking Ability Can arise from neurological injury or disease as well as in advancing age. May be subtle or extreme changes in remembering, thinking or temperament. | Keep your brain stimulated with conversation, thinking, socialization, etc. Be a part of life. | Therapeutic intervention can be obtained to assist the individual with their specific needs. Keep a notepad handy for recording important information. A calendar will assist with keeping track of activities. Use reminders posted in the environment. |
| Dementia A range of symptoms that affect cognitive function. It may occur with neurological disease or as a consequence of neurological injury. Occurs most often in older individuals but can be evident at any age with neurological issues. | Monitor for signs of forgetfulness, confusion. | Use cues such as a daily schedule. Write information that needs to be remembered. Remind the individual or set an alarm for toileting time. Seek early medical intervention. |
| Stress and Anxiety Neurologic injury or disease disrupts life. | Practice stress reduction techniques. Prepare for activities ahead of time to reduce unknown events. Speak up to have your needs met. | Seek treatment advice from a peer mentor, mental health professional, or healthcare professional. Medications can help. |
| Depression A medical condition that affects brain chemical balance. | Eat a well-balanced diet. Move your body or have someone move the body parts that you cannot move. Plan activities with others. Enjoy the outdoors. | Seek advice from a mental health professional for techniques to counter depression. A mental health professional can assist with building strategies for the future. Medications can assist with treatment. |
| Detailed Spasticity information can be found here. Detailed Neurogenic Pain information can be found here. | ||
Cardiovascular System (Heart and Blood Vessels)
The heart serves as a pump to keep blood flowing through the arteries and veins. Some individuals will inherit a genetic risk of heart disease. Individuals who are older have a higher risk of heart disease due to lifestyle. Cardiac issues are also a risk factor in individuals with paralysis, especially due to inactivity and sedentary lifestyle.
Diet and mobility are key factors in maintaining cardiovascular health at any age. Be sure to include movement to parts of your body that are affected by paralysis in addition to your whole body. Follow the instructions provided by your healthcare professional for cardiac issues.
| Cardiovascular System (Heart and Blood Vessels) with Aging and Paralysis | Prevention | Intervention |
| Autonomic Dysreflexia (AD) A sudden increase in an individual’s normal blood pressure is usually the primary symptom. Occurs at any time in those with some head injuries, and those with spinal cord injury above T6-T10. | Measure blood pressure at various times and with various activities to determine your individual blood pressure and to diagnose AD and silent AD. If triggers are identified, avoid them. | Quickly have someone sit you bolt upright to drop blood pressure. Check bladder and urinary equipment, then check bowel for impaction or diarrhea, then skin for irritations. Look for anything that may be upsetting your body below the level of injury. Call 911 if needed. |
| Orthostatic Hypotension (OH) A sudden drop in blood pressure typically when changing to a sitting or standing position. Occurs most often in the acute phase of injury, with progression of disease, or if new equipment is introduced that changes your position from sitting to standing. Increased episodes of OH can occur with aging as arteries can become stiff. | Return to a lying position. Elevate more slowly. Resolves over time but may return as arteries become thicker with age. Use elastic stockings and an abdominal binder to assist with blood flow return. Provide movement to legs and arms. | Change positions slowly. Monitor blood pressure with OH when changing positions to detect lower blood pressure and increase position slowly. Medication may assist with persistent issues. |
| Edema Occurs at any time after paralysis, but may be increased with age as arteries might become less elastic. | Elevate legs higher than the heart when possible, to enable blood flow return. Use elastic stockings to assist with edema control. | Notify your healthcare professional if the edema increases. Medication may be needed. Check the lower back for increased fluid collection. |
| Deep Vein Thrombosis (DVT) (blood clot) Occurs at any time with paralysis, may have an increased risk with age. | DVT can appear in the legs, arms, or other parts of the body. May or may not sense pain. May have a color change on the skin, and/or swelling. Do not rub the area; this can release the clot. Can occur anytime but increases in those over 40 years. | Use compression arm sleeves, stockings, and abdominal binders. Avoid pressure on joints from equipment, ‘hooking’ an arm on the back of a wheelchair, or crossing legs. Medication or surgery may be required. |
| Low blood pressure Occurs at any time with paralysis, may be counteracted as the body ages, with arteries becoming less elastic. | Monitor your blood pressure during various activities so you are aware of your average. | Medication for low and high blood pressure is available. Work with your healthcare professional to find the right treatment specifically for you. |
| Irregular heartbeat May occur at any time with paralysis, may be increased risk with normal aging. | Monitor your pulse for an even beat and flow. Notify your healthcare professional if you notice an uneven, unprovoked faster or slower pulse. Eat well Monitor your weight Stop smoking Exercise Practice stress reduction | Medication or cardiac implant, such as a pacemaker, may be required. |
| Atherosclerosis May occur at any time with paralysis, may be increased risk with normal aging. | Keep regular wellness check-ups with your healthcare professional. Eat well Monitor your weight Stop smoking Exercise Practice stress reduction | Medication may be prescribed. |
| Inactivity Less movement to the area of paralysis can increase health issues at an earlier age or increase existing health conditions at a later age. | Slowly start an exercise program that includes the paralyzed parts of your body. Keep your mind active. | Find activities that interest you that include movement. |
| Detailed Autonomic Dysreflexia can be found here. Deep Vein Thrombosis information can be found here. Find AD and DVT wallet cards here. | ||
Endocrine System (Hormones)
The chemical functioning of your body is controlled in the brain with messages being sent by the endocrine system. This keeps the body functioning in harmony. Hormones can be affected by paralysis but generally, it is temporary.
| Endocrine System (Hormones) with Aging and Paralysis | Prevention | Interventions |
| Diabetes Type I diabetes and diabetes insipidus can occur with neurological issues. Type II diabetes can occur as a secondary complication due to aging, lifestyle, and/or neurological issues. | Maintain a healthy diet and weight. Move your body. This assists with muscle metabolism. Monitor your fluid intake balancing it with your bladder management program. | Diabetes can be controlled by a combination of diet, exercise, careful monitoring, and medication. It is important to monitor your condition to control blood glucose. Eat a balanced diet, in moderation. Stop smoking. Decrease intake of alcohol and sugary drinks. |
| Low Testosterone Males with low production of the hormone, testosterone leading to decreased sex drive, erectile dysfunction, fatigue, irritability, depression, decreased hair, muscle, bone mass, and increased body fat. May occur with aging or neurological issues. | Exercise regularly, even the part of your body that needs assistance. Establish a regular sleep pattern. Manage stress. Limit alcohol. Stop smoking and other inhalants and recreational drugs. | Medication may be needed to balance your testosterone levels. Avoid over the counter testosterone supplements that may not be what your body requires. |
| Sexual Function Due to lack of motor control and/or sensation from neurological injury, sexual function and sexual drive may be diminished. Also, may occur due to aging issues. | Choose a partner that is willing to share your unique experience. Explore on your own or with a partner. Use your mind. Explore positions. Use lubricant. | Therapists are available that can provide information about positioning. Videos from reliable sources such as major rehabilitation facilities can provide safe ideas. Erectile medications for males are available. |
| Menstruation In women, menstruation may decrease or temporarily pause with neurological issues. The average age for cessation of menstruation is 55 years. | Variation in cycles and flow may occur. Temporary halting of menstruation may occur. Use birth control if not planning pregnancy. | Cycles usually spontaneously resume if menopause has not occurred. |
| Perimenopause/Menopause Onset varies with age, genetics, and neurological injury. Changes may affect sexual function. | Variations in cycles may occur. Use lubricant during sex. | Medical treatments are available to reduce symptoms, if needed. |
| Pregnancy For some women, pregnancy may be difficult to achieve, increased difficulty may occur with neurological disease. Men may not be able to ejaculate. | Birth control should be used if pregnancy is not desired. | Invitro fertilization may be used. Retrieving sperm medically is possible. |
| More information about sexual health can be found here. | ||
Respiratory System (Breathing)
Breathing can be affected by paralysis. Lack of movement on one side of the body can affect the ability of the lung to expand and contract. Paralysis on both sides of the body affects both lungs. The ability to have a forceful cough to expel mucous or other blockage leaves the body open to infection in the lungs such as pneumonia. There can also be an increased risk of infection if mechanical ventilation is used.
Breathing uses muscles around the rib cage, abdominal muscles and even muscles in the shoulders and back, among others. As individuals age, just as chest muscles become less elastic like the other muscles in the body, lung tissue becomes less elastic making it more challenging to breathe, clear your throat, and cough.
Performing pulmonary exercises such as deep breathing and coughing exercises can assist with keeping your lungs and breathing muscles functioning. Starting at the time of the onset of paralysis or even before with a general exercise program helps keep your lungs healthy.
Smoking and other non-medical inhalants rob your lungs of oxygen that is needed for body functions. Nicotine and other substances that should not be in the body will pass through your lungs blocking the oxygen molecules that are needed for health. Your healthcare professional can provide treatments to help you stop smoking.
| Respiratory System (Breathing) with Aging and Paralysis | Prevention | Intervention |
| Deep Breathing Many muscles in the body are used for breathing. These can both be weakened by aging and paralysis. | Avoid individuals who have temporary respiratory health issues such as a cold, flu or other. Wash your hands. | Practice taking three deep breaths and coughing several times a day to expand and clear lungs. Therapy can assist with techniques to help with deep breathing and clearing your lungs. Follow treatments for spasticity (tone). |
| Assisted Breathing Mechanical assistance can help breathing which can be affected by some neurological issues. Weakened muscles from aging can increase your need for breathing assistance. | Use the mechanical ventilation cough assist feature to help clear lungs. | Check with your healthcare professional to see if you can use internal or external mechanical ventilation. Diaphragmatic pacemakers can assist with removal of mechanical ventilation of some individuals. |
| Lung Infections Due to weak muscles from aging and neurological issues, deep breathing, and the ability to cough can be affected. This can lead to infections in the lungs. | Practice coughing and deep breathing either on your own or with mechanical assistance. Note any changes in color of your sputum. It should be clear. Change positions frequently. Monitor temperature if you suspect an infection. Keep up with annual immunizations. | Therapeutic techniques can help clear your lungs. Notify your healthcare professional for medical treatment if you suspect an infection. |
Gastrointestinal System (Stomach and Bowel)
Digestion and elimination are issues for individuals with aging and neurological concerns. In aging, functions of the body may slow. This can impact the swiftness of digestion and elimination. It can take longer for contents to pass through the stomach and bowel. Gallstones form more easily. The longer stool is in the bowel, the more fluid is removed leading to constipation. Hard stools can lead to hemorrhoids and fissures.
Neurological issues lead to the same digestive and elimination problems, but slowness of the bowel is caused by decreased nerve function and mobility challenges. This is neurogenic bowel. The source is a miscommunication of the nerves. With neurological injury, the health issue is neurogenic bowel. Constipation can still occur but treating constipation alone will not help treat neurogenic bowel. A bowel program is the treatment for neurogenic bowel.
A combination of nerve function slowing and aging leads to more difficulty. Individuals who develop paralysis as younger individuals start their bowel program and typically have success. However, there may be a sudden or slow change with aging that makes the bowel program more difficult after years of success.
| Gastrointestinal System (Stomach and Bowel) with Aging and Paralysis | Prevention | Intervention |
| Feeling full Your stomach may feel full longer due to the slow passage of food. | Eat smaller portions. Chew well so the stomach has less need to break down your food. Have small, more frequent meals. Sit upright, if possible while eating. Avoid foods that produce gas. | Move your lower body to help stimulate the bowel muscles to work. Walk after eating, if able. |
| Gallstones Slowness in the gut due to nerve issues or aging, prevents the gallbladder from releasing bile in a timely manner. | Symptoms of gallstones may not be recognized with paralysis. There may be increased spasticity, autonomic dysreflexia, referred pain to shoulder or jaw, or just a feeling that something is wrong. Avoid foods that contain high-fat, eggs, sweets, fried foods, refined foods, soda and alcohol, among others. | Treatments range from observation to surgical interventions. |
| Neurogenic bowel A nerve issue in the bowel that slows function. It may not be noticed in younger individuals with paralysis but aging typically changes the swiftness of the bowel program. | Incorporate foods high in roughage into your dietary routine. Follow your prescribed bowel program. | Maintain a strict schedule to perform the bowel program. Drink water in accordance with your bladder management program. Learn to sit upright to let gravity assist with the bowel program. |
| Hemorrhoids Enlarged veins in the lower rectum. | Generously use lubricant during the bowel program. Bleeding may be the first sign of hemorrhoids. | Ask your healthcare professional about use of stool softener. If hemorrhoids appear, gently return them to the inside of the bowel with a gloved, well lubricated finger. Notify your healthcare professional to assess if further treatment is required. Surgical options may be needed. |
| Impaction Hard stool in the bowel that cannot be passed with a bowel program. | Incorporate foods high in roughage into your dietary routine. Follow your prescribed bowel program. Move your lower body several times a day or have someone move it for you to stimulate bowel function. Vomiting stool is an advanced sign of impaction and requires immediate medical attention. | A low impaction may be manually removed. Watch for symptoms of autonomic dysreflexia. Impactions may need to be removed by medical personnel. |
| Detailed information about bowel care can be found here. | ||
Urinary System (Kidneys and Bladder)
The kidneys and bladder work together to remove fluid waste from the body. The kidneys (upper urinary system) filter waste from the blood stream creating urine. This fluid flows down the ureters to the bladder (lower urinary system) which stores the urine until time to expel it from the body.
Aging can lead to slight bladder shrinking which makes toileting more frequent. The sensation of the need to toilet may be weaker and the sphincters that control urine may become weaker, so getting to the toilet can be an issue. Mobility problems can lead to difficulty in manipulation of clothing in time to toilet.
Neurological issues lead to either incontinence (accidental release of urine) or an inability to expel urine. This is due to neurogenic bladder which is an issue with nerve communication. It requires different treatment than bladder issues with aging.
Both aging and a neurogenic bladder can lead to similar issues but treatments are different.
| Urinary System (Kidneys and Bladder) | Prevention | Intervention |
| Infection Can be in the bladder or kidneys or both. | Drink water within the parameters of your blader management program. Avoid overuse of alcohol, sugared or artificially sugared drinks, caffeinated drinks. Move your legs or have someone move them which shakes the contents of the bladder so bacteria have less chance of clumping together. Wash your hands prior and after toileting or performing your bladder program. Clean yourself well after toileting. | If an infection is suspected, have a urinalysis and culture test to determine the specific bacteria in your urine. Antibiotic treatment should be matched to the specific bacteria. |
| Neurogenic Bladder Caused by miscommunication of the nerves in bladder control. In addition to removing urine, the sphincters of the bladder may fail to work in unison. | Wash your hands prior and after toileting or performing your bladder program. Clean yourself well after toileting. Exercise your body. | Strictly follow your bladder program. Have your bladder program modified if leaking. Obtain urodynamic testing to ensure your lower urinary system is functioning properly. |
| Pressure Injury Can be caused by urine leaking. | Keep your body clean and dry. Avoid wearing pads that will keep urine on the skin. | Follow the prescribed treatment for your pressure injury. Stay off the area until healed. |
| Detailed information about bladder management can be found here. | ||
Lymphatic and Immune System (Infection fighting)
The immune system control’s reaction to infection and other pathogens. Both aging and neurological injury can affect the effectiveness of the immune system. Pathogens may not be recognized, recognized in a timely manner, or reacted to by the immune system. This can make healing from infections more challenging.
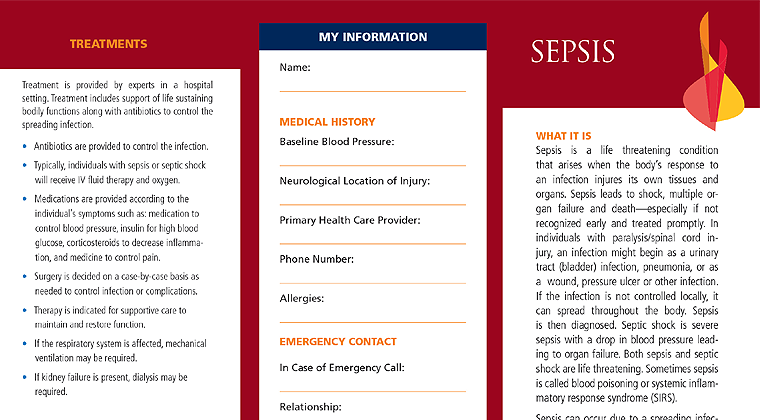
Sepsis is an infection that occurs after an initial infection. You may have had a slight infection that was so slight that you did not even notice it or it can evolve from a significant infection. This is a medical emergency. It is more often found in aging and with neurological issues but can come at any time and at any age.
| Lymphatic and Immune System (Infection fighting) | Prevention | Intervention |
| Infection An overdevelopment of germs and viruses anywhere in the body. Paralysis can affect the body’s ability to fight germs. | Wash your hands carefully. Note changes in your body. Examine all parts of your body as you may not feel an infection starting. Cover scratches or small wounds. Manage stress. Stay up to date with vaccinations. | Seek medical attention if a wound shows signs of infection development. |
| Sepsis A medical emergency when the body has an extreme reaction to an infection. Often it appears after an initial infection that you thought was healed but later flares up again. This is a life-threatening issue. | Note symptoms of confusion, rapid breathing, or pain. Call 911. Tell all health professionals dealing with this episode that you think you have sepsis. Print several copies of the Christopher & Dana Reeve Foundation Sepsis Wallet Card and give it to everyone treating you. | Emergency medical treatment is needed to prevent complications of sepsis. |
| Detailed information about sepsis can be found here. Find sepsis wallet cards here. | ||
How to Diagnose a Health Issue
You may be the first person to recognize a potential health issue in your body.
The owner and responsible party for your body is you! If you sense something is wrong in your body, check to establish what it may be. For example, you may see something like a blister on your foot or a pigment change on the skin of your hip. Take action to ensure healing.
Be sure to look for any issues that you cannot sense or feel. This may include looking at your body with a mirror to see all areas. Even if someone looks for you, it is critical that you see for yourself what is occurring.
Gaining knowledge about paralysis is an important skill to know what you are facing and how to deal with health issues. Some basic life skills will be done differently. Being able to care for yourself today will help reduce the risks of aging. Referred pain is a start to locating the actual source of the issue.
With sensation changes, it may be challenging to know discomfort or pain. With paralysis, pain may be referred to the arm, upper back, jaw or a location where you have sensation. Never ignore pain. It is a signal that something is not right inside your body.
Know your ‘normals’ such as your average blood pressure, heart rate, temperature, color, smell, amount of your urine and stool, state of your skin, swallowing ability and changes, breathing issues, etc. Recognize when something is wrong or just feels ‘off’.
Others can assist with diagnosis of health issues.
To maintain health while aging with paralysis and aging into paralysis, be sure to keep your medical, dental, and specialty appointments. Establish a routine with health providers who are knowledgeable about your condition. These individuals will follow your general medical condition, alert you to issues that may become health concerns, and suggest testing and treatments that are needed to prevent major issues from occurring.
The mouth is the gateway into the body. Dental care is critical to maintaining health in being able to chew and preventing infection. Research has demonstrated that good oral hygiene is essential, especially in cardiac health, a complication that can occur with paralysis. Your dentist can enable you to ensure long-term health.
Mental well-being is an issue for individuals with paralysis. As aging occurs or barriers are confronted, having the skills to notice and prepare for challenges can help you make good choices and deal with issues. Checking in with a counsellor or therapist who is knowledgeable about issues with paralysis can assist with dealing with today and planning for the future.
Healthcare specialists are needed to deal with issues that arise from paralysis. This can include medical physicians, surgeons, dentists, psychologists, registered nurses, physical therapists, occupational therapists, speech and language pathologists, respiratory therapists, podiatrists, home health professionals, vocational counselors, reproductive specialists, among many others. Some of these individuals will be seen on a regular basis, while others will be episodic. Not everyone will need all these services. Most individuals will require only a few specialists, a few others may need none.
When testing is ordered for any health issue, be sure to follow up with getting that work completed. The sooner you complete your testing; the sooner early interventions can be provided. The earlier treatment begins, the less time will be needed to remedy this health issue or to provide essential treatments.
How to Treat Health Conditions
Care for any health condition is best provided as soon as possible. Waiting out a health concern may make treatment more difficult and complicated. A brief review of possible preventions and interventions (treatments) are listed in the charts above.
Polypharmacy is a situation where an individual takes multiple medications every day. Typically, it is more than five or more different medications, Individuals should be sure to know what each medication is treating, the side effects, and contraindications. Often, when seeing multiple providers for different issues, medications may be prescribed that interact with each other or counteract when taken together. Be sure to report all medications, over the counter supplements, recreational drugs, inhalants, lotions, or any other substances that are ingested, inserted, inhaled, or rubbed on the body to ensure there are no reactions or duplicate treatments.
The Model Knowledge Translation Center offers an infographic that provides information about aging successfully with spinal cord injury. These tips can be used by anyone with paralysis.
What are Some Rehabilitation and Therapies
The type of rehabilitation and therapies needed are unique to each individual and their life stage.
• As you and your caregiver age, additional supportive equipment, especially for moving your body may be available to you.
• Your payor may provide two weeks of mobility training per year to advance your therapy. This is typically outpatient and does not have to be sequential days. It must be ordered by your healthcare professional. Check your policy to see if you are eligible.
• If you are looking for support from someone in the same situation, consider the Christopher & Dana Reeve Foundation’s Peer and Family Support Program or try a virtual support group.
What are Some Facts and Figures
Results of a national paralysis survey concerning aging with and aging into paralysis were published in 2016 by Dixon-Ibarra, Krahn, Fredine, Cahill, & Jenkins, (Adults Aging ‘with’ and ‘into’ Paralysis: Epidemiological Analyses of Demography and Health. Disability and Health Journal, 9(4), 575-583. https://doi.org/10.1016/j.dhjo.2016.06.003) and the results indicated:
• Of the individuals aging with paralysis, 80% had disabilities for 40+ years, had better self-reported health status, and a trend for more secondary and medical conditions.
• Individuals aging into paralysis had more chronic diseases.
Resources
If you are looking for more information about aging with paralysis and aging into paralysis or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 7:00 am to 8:00 pm EST.
Additionally, the Reeve Foundation maintains fact sheets on aging. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
Model System Knowledge Translation Center (MSKTC) which provides information for those with spinal cord injuries, traumatic brain injuries, and burns. MSKTC has a factsheet on aging with spinal cord injury.
Each state in the U.S. has an Agency on Aging and Disability. US Aging provides more information on them. Check your state’s government listings.
References
Acquarone E, Monacelli F, Borghi R, Nencioni A, Odetti P. Resistin: A Reappraisal. Mech Aging Dev. 2019 Mar;178:46-63. doi: 10.1016/j.mad.2019.01.004. Epub 2019 Jan 14. PMID: 30650338.
Annweiler C, Schott AM, Berrut G, Chauviré V, Le Gall D, Inzitari M, Beauchet O. Vitamin D and Aging: Neurological Issues. Neuropsychobiology. 2010 Aug;62(3):139-50. doi: 10.1159/000318570. Epub 2010 Jul 14. PMID: 20628264.
Bauman WA, Spungen AM, Adkins RH, Kemp BJ. Metabolic and Endocrine Changes in Persons Aging with Spinal Cord Injury. Assist Technol. 1999;11(2):88-96. doi: 10.1080/10400435.1999.10131993. PMID: 11010069.
Beuret-Blanquart F, Boucand MH. Vieillissement chez les blessés médullaires [Aging with Spinal Cord Injury]. Ann Readapt Med Phys. 2003 Dec;46(9):578-91. French. doi: 10.1016/j.annrmp.2003.05.002. PMID: 14642669.
Bohr VA, Ottersen OP, Tønjum T. Genome Instability and DNA Repair in Brain, Aging and Neurological Disease. Neuroscience. 2007 Apr 14;145(4):1183-6. doi: 10.1016/j.neuroscience.2007.03.015. Epub 2007 Apr 2. PMID: 17400394.
Dixon-Ibarra, A., Krahn, G., Fredine, H., Cahill, A., & Jenkins, S. (2015). Epidemiology Health of Adults “Aging With” vs “Aging Into” Disability: National Paralysis Survey 2012-2013. The Gerontologist, 55(Suppl_2), 96. https://doi.org/10.1093/geront/gnv500.01
Dixon-Ibarra, A., Krahn, G., Fredine, H., Cahill, A., & Jenkins, S. (2016). Adults Aging ‘with’ and ‘into’ Paralysis: Epidemiological Analyses of Demography and Health. Disability and Health Journal, 9(4), 575-583. https://doi.org/10.1016/j.dhjo.2016.06.003
Dolbow DR, Gorgey AS, Daniels JA, Adler RA, Moore JR, Gater DR Jr. The Effects of Spinal Cord Injury and Exercise on Bone Mass: A Literature Review. NeuroRehabilitation. 2011;29(3):261-9. doi: 10.3233/NRE-2011-0702. PMID: 22142760.
Fulop T, Dupuis G, Baehl S, Le Page A, Bourgade K, Frost E, Witkowski JM, Pawelec G, Larbi A, Cunnane S. From Inflamm-Aging to Immune-Paralysis: A Slippery Slope During Aging for Immune-Adaptation. Biogerontology. 2016 Feb;17(1):147-57. doi: 10.1007/s10522-015-9615-7. PMID: 26472173.
Groah SL, Charlifue S, Tate D, Jensen MP, Molton IR, Forchheimer M, Krause JS, Lammertse DP, Campbell M. Spinal Cord Injury and Aging: Challenges and Recommendations for Future Research. Am J Phys Med Rehabil. 2012 Jan;91(1):80-93. doi: 10.1097/PHM.0b013e31821f70bc. PMID: 21681060.
Grosboillot N, Gallou-Guyot M, Lamontagne A, Bonnyaud C, Perrot A, Allali G, Perrochon A. Towards a Comprehensive Framework for Complex Walking Tasks: Characterization, Behavioral Adaptations, and Clinical Implications in Aging and Neurological Populations. Aging Res Rev. 2024 Nov;101:102458. doi: 10.1016/j.arr.2024.102458. Epub 2024 Aug 15. PMID: 39153599.
Guízar-Sahagún G, Grijalva I, Franco-Bourland RE, Madrazo I. Aging with Spinal Cord Injury: A Narrative Review of Consequences and Challenges. Aging Res Rev. 2023 Sep;90:102020. doi: 10.1016/j.arr.2023.102020. Epub 2023 Jul 23. PMID: 37487887.
Hurley MJ, Bates R, Macnaughtan J, Schapira AHV. Bile Acids and Neurological Disease. Pharmacol Ther. 2022 Dec;240:108311. doi: 10.1016/j.pharmthera.2022.108311. Epub 2022 Nov 16. PMID: 36400238.
Jiang SD, Dai LY, Jiang LS. Osteoporosis After Spinal Cord Injury. Osteoporos Int. 2006 Feb;17(2):180-92. doi: 10.1007/s00198-005-2028-8. Epub 2005 Oct 11. Erratum in: Osteoporos Int. 2006;17(8):1278-81. PMID: 16217589.
Jörgensen S, Hedgren L, Sundelin A, Lexell J. Global and Domain-Specific Life Satisfaction Among Older Adults with Long-Term Spinal Cord Injury. J Spinal Cord Med. 2021 Mar;44(2):322-330. doi: 10.1080/10790268.2019.1610618. Epub 2019 May 17. PMID: 31099721; PMCID: PMC7952060.
Kandogan T, Seifert E. Influence of Aging and Sex on Voice Parameters in Patients with Unilateral Vocal Cord Paralysis. Laryngoscope. 2005 Apr;115(4):655-60. doi: 10.1097/01.mlg.0000161344.23128.9d. PMID: 15805876.
Kikura M, Suzuki K, Itagaki T, Takada T, Sato S. Age and Comorbidity as Risk Factors for Vocal Cord Paralysis Associated with Tracheal Intubation. Br J Anaesth. 2007 Apr;98(4):524-30. doi: 10.1093/bja/aem005. Epub 2007 Mar 6. PMID: 17341543.
McColl MA, Charlifue S, Glass C, Savic G, Meehan M. International Differences in Aging and Spinal Cord Injury. Spinal Cord. 2002 Mar;40(3):128-36. doi: 10.1038/sj.sc.3101264. PMID: 11859439.
McMurran CE, Wang Y, Mak JKL, Karlsson IK, Tang B, Ploner A, Pedersen NL, Hägg S. Advanced Biological Aging Predicts Future Risk for Neurological Diagnoses and Clinical Examination Findings. Brain. 2023 Dec 1;146(12):4891-4902. doi: 10.1093/brain/awad252. PMID: 37490842; PMCID: PMC10690013.
Muensterer OJ. Hyperkalaemic Paralysis. Age Aging. 2003 Jan;32(1):114-5. doi: 10.1093/aging/32.1.114. PMID: 12540358.
Paramanik V, Kurrey K, Singh P, Tiwari S, Nisha. Roles of Genistein in Learning and Memory During Aging and Neurological Disorders. Biogerontology. 2023 Jun;24(3):329-346. doi: 10.1007/s10522-023-10020-7. Epub 2023 Feb 25. PMID: 36828983.
Pfalzer AC, Bowman AB. Relationships Between Essential Manganese Biology and Manganese Toxicity in Neurological Disease. Curr Environ Health Rep. 2017 Jun;4(2):223-228. doi: 10.1007/s40572-017-0136-1. PMID: 28417441; PMCID: PMC5515274.
Sabariego C, Ehrmann C, Bickenbach J, Pacheco Barzallo D, Schedin Leiulfsrud A, Strøm V, Osterthun R, Tederko P, Seijas V, Eriks-Hoogland I, Le Fort M, Gonzalez Viejo MA, Bökel A, Popa D, Dionyssiotis Y, Baricich A, Juocevicius A, Amico P, Stucki G. Aging, Functioning Patterns and Their Environmental Determinants in the Spinal Cord Injury (SCI) Population: A Comparative Analysis Across Eleven European Countries Implementing the International Spinal Cord Injury Community Survey. PLoS One. 2023 Apr 20;18(4):e0284420. doi: 10.1371/journal.pone.0284420. Erratum in: PLoS One. 2025 Nov 25;20(11):e0337486. doi: 10.1371/journal.pone.0337486. Erratum in: PLoS One. 2025 Dec 2;20(12):e0337859. doi: 10.1371/journal.pone.0337859. PMID: 37079622; PMCID: PMC10118153.
Sendzischew Shane MA, Moshiree B. Esophageal and Gastric Motility Disorders in the Elderly. Clin Geriatr Med. 2021 Feb;37(1):1-16. doi: 10.1016/j.cger.2020.08.002. Epub 2020 Oct 29. PMID: 33213764.
Smith DL, Akhtar AJ, Garraway WM. Proprioception and Spatial Neglect After Stroke. Age Aging. 1983 Feb;12(1):63-9. doi: 10.1093/aging/12.1.63. PMID: 6846094.
Szeto RA, Tran T, Truong J, Negraes PD, Trujillo CA. RNA Processing in Neurological Tissue: Development, Aging and Disease. Semin Cell Dev Biol. 2021 Jun;114:57-67. doi: 10.1016/j.semcdb.2020.09.004. Epub 2020 Oct 16. PMID: 33077405; PMCID: PMC8050165.
van Domburg PH, ten Donkelaar HJ. The Human Substantia Nigra and Ventral Tegmental Area. A Neuroanatomical Study with Notes on Aging and Aging Diseases. Adv Anat Embryol Cell Biol. 1991;121:1-132. PMID: 2053466.
Verkhratsky A, Zorec R, Rodriguez-Arellano JJ, Parpura V. Neuroglia in Aging. Adv Exp Med Biol. 2019;1175:181-197. doi: 10.1007/978-981-13-9913-8_8. PMID: 31583589; PMCID: PMC7188603.
Villemagne VL, Okamura N. Tau Imaging in the Study of Aging, Alzheimer’s Disease, and Other Neurodegenerative Conditions. Curr Opin Neurobiol. 2016 Feb;36:43-51. doi: 10.1016/j.conb.2015.09.002. Epub 2015 Sep 20. PMID: 26397020.
Warren NM, Burn DJ. Progressive Supranuclear Palsy. Pract Neurol. 2007 Feb;7(1):16-23. PMID: 17430861.
Weitzenkamp DA, Jones RH, Whiteneck GG, Young DA. Aging with Spinal Cord Injury: Cross-Sectional and Longitudinal Effects. Spinal Cord. 2001 Jun;39(6):301-9. doi: 10.1038/sj.sc.3101146. PMID: 11438851.
Wirz M, Dietz V. Concepts of Aging with Paralysis: Implications for Recovery and Treatment. Handb Clin Neurol. 2012;109:77-84. doi: 10.1016/B978-0-444-52137-8.00005-X. PMID: 23098707.
Xu T, Ye J, Gan L, Deng S, Guo Y, Tang Y. Advancing Neurological Health: Insights into Aging, Immunity, and Vascular Dynamics. Aging Dis. 2024 May 7;15(3):939-944. doi: 10.14336/AD.2024.0423. PMID: 38722789; PMCID: PMC11081148.
Young BM, Williams J, Prabhakaran V. BCI-FES: Could a New Rehabilitation Device Hold Fresh Promise for Stroke Patients? Expert Rev Med Devices. 2014 Nov;11(6):537-9. doi: 10.1586/17434440.2014.941811. Epub 2014 Jul 25. PMID: 25060658; PMCID: PMC4194138.
Zhang W, Huang C, Yao H, Yang S, Jiapaer Z, Song J, Wang X. Retrotransposon: An Insight into Neurological Disorders from Perspectives of Neurodevelopment and Aging. Transl Neurodegener. 2025 Mar 25;14(1):14. doi: 10.1186/s40035-025-00471-y. PMID: 40128823; PMCID: PMC11934714.